Booster waning, Long Covid brain fog, and potential of Paxlovid resistance
Daily update #7, 9 November 2022
A relatively quiet day on the Covid front, which is good.
Three papers of note.
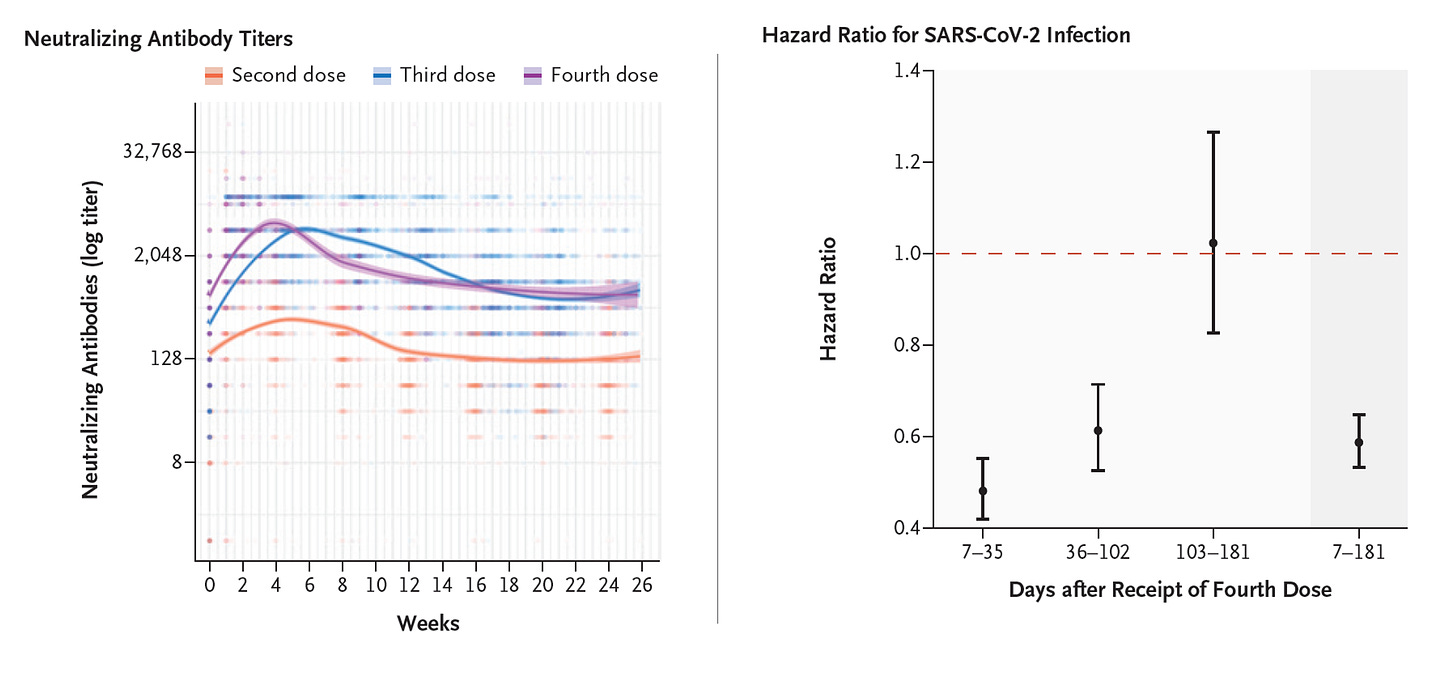
First, from Israel, a 6-month follow up of over 11,000 health care workers who had received a 4th dose of mRNA (Pfizer) vaccine. There was a good neutralizing antibody response, as strong as the 1st booster, but more rapid falloff of protection vs infection, lasting just over 3 months (~100 days)(Figure below). One more study that goes against the notion of an annual Covid shot. From other recent reports, there has also been some slippage of protection vs severe Covid (i.e. hospitalizations and deaths), but that has held up far better (consistently >75% vaccine effectiveness) than against infections. On a more optimistic note, a new review on mRNA vaccines published today demonstrated the marked potential to tweak the mRNA-nanoparticle platform to improve delivery efficiency, durability of efficacy, and reduce the side-effects (reactogenicity). The question is why this is not being aggressively pursued for next generation Covid vaccines which could be more effective, better tolerated, and potentially have at least 1 year of durable protection.
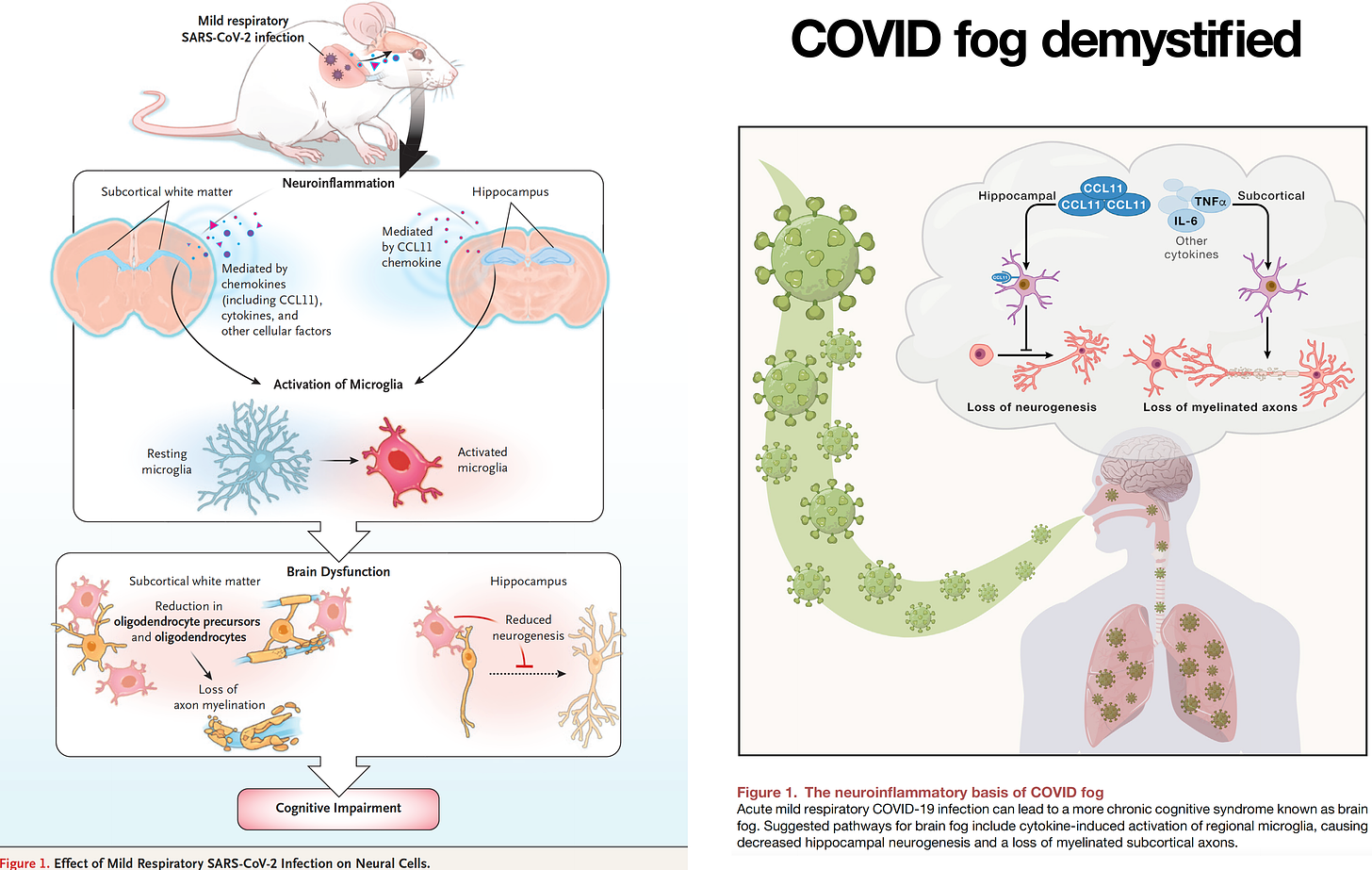
Second, a mechanistic review of what we know about brain fog after a mild covid infection. It’s a recap of a paper published in June using a mouse model and recapitulated in a small group of patients. Neuroinflammation was induced and while there was no evidence of direct virus infection, the microglia was activated in brain white matter, with subsequent loss of myelin. The inflammation seen in the hippocampus may explain the clinical symptoms of memory impairment. A biomarker of inflammation—CCL11—was increased in the model and in patients suffering Long Covid with brain fog. It should be considered a candidate to track the process along with potential therapies, such as targeting microglial activation— well worth a clinical trial. There is an FDA approved drug (Pexidartinib) that potentially could be repurposed for such a trial.
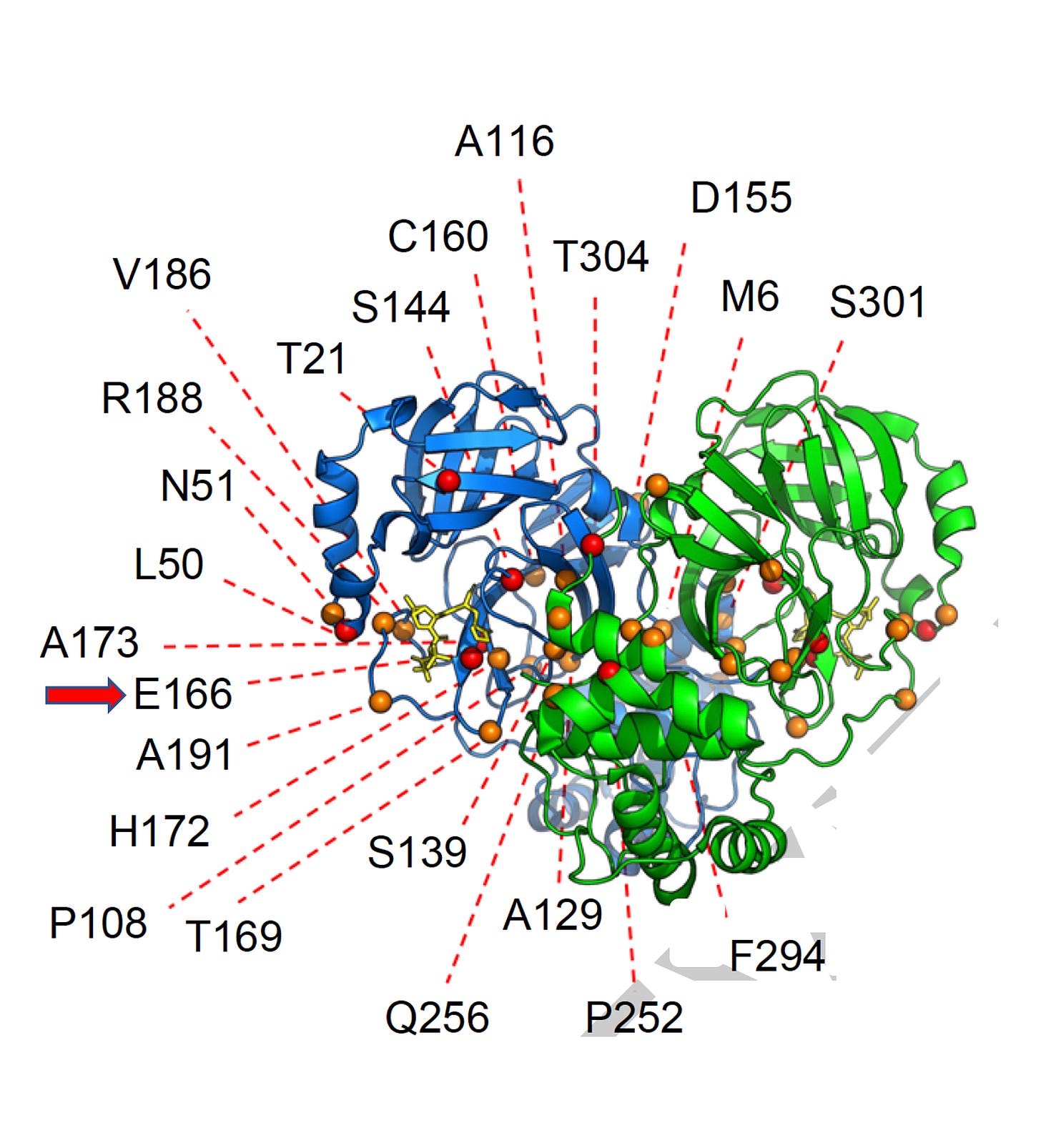
Third, the Ho lab published in Nature multiple pathways that could lead to Paxlovid resistance—something we surely do not want to see in the clinic. These were not naturally occurring mutations in the virus’s main protease, the target of Paxlovid (other studies have reported some that have been seen in people) but were induced in the lab. One in the new study at the E166 site had ~100-fold resistance. While the findings are in lab, not clinical, we presently have no backup for Paxlovid. The new variants such as BQ.1.1 and XBB have already overridden our monoclonal antibody treatments. Along with several other reports about the potential for Paxlovid resistance to emerge, much stronger efforts to accelerate new oral drugs, and combinations are needed.
There was yet another mask study to show how Covid infections cropped up substantially in schools in Massachusetts when the universal mask policy was rescinded. I will never understand the people (including physicians) who continually and vehemently try to debunk the utility of masks (particularly those of high quality, fitted, worn properly) to inhibit a respiratory virus.
That’s it for today. Thanks for reading and a reminder that your free subscription will insure you get the newsletter directly to your email.