Long-Term Long Covid
New reports at two years and the known unknowns that lie ahead
Today there are 2 new papers published on the 2-year follow up of over 100,000 people with Covid and millions of uninfected controls. In this edition of Ground Truths, I’ll review the salient findings of the 2 studies, and highlight the uncertainties of our knowledge base for Long Covid, which has already compromised the lives of tens of millions of people. Unfortunately, what was seen at 6 months largely continues out to 2 years.
The Sequelae Paper
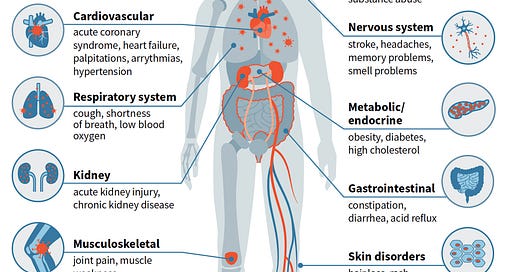
Ziyad Al-Aly and colleagues have published multiple seminal papers on Covid outcomes from the large Veterans Affairs dataset throughout the pandemic and this new one at Nature Medicine addresses what happened 2 years later to nearly 140,000 people who had Covid, compared with almost 6 million people non-infected controls. Of those with Covid, 118,238 were not hospitalized and 20,580 were hospitalized. The authors pre-specified 80 different sequelae, categorized into 10 organ systems, as shown below. It is the first systematic study of adverse outcomes at the 2-year mark after Covid.
The authors imputed disability-adjusted life years (DALYs) by calculating the product of the incident rate (by organ system) times the health burden coefficient (reviewed in Supplementary Table 16). If you’re not familiar with DALY, it’s the most accepted metric of overall disease burden, expressed as the number of years lost due to ill-health, disability or early death. You can see from the top graph (a) the percentage of cumulative DALYs and in the lower graph (b) per 1,000 persons. Note the X-axis in lower graph b is very different for non-hospitalized compared with hospitalized. The lighter color shades refer to the 1st year post-Covid; the darker correspond to the 2nd year. For both groups of people, the toll of adverse sequelae were worst during the first year.
The major finding is that the people with severe Covid, who were hospitalized, had worse outcomes and DALYs as compared with those individuals with mild to moderate Covid, not hospitalized. But in the non-hospitalized group a substantial proportion— about 30%— of the 80 sequelae, including GI and neurologic, remained significantly elevated. About 20% of DALYs were attributable to the second year in both groups.
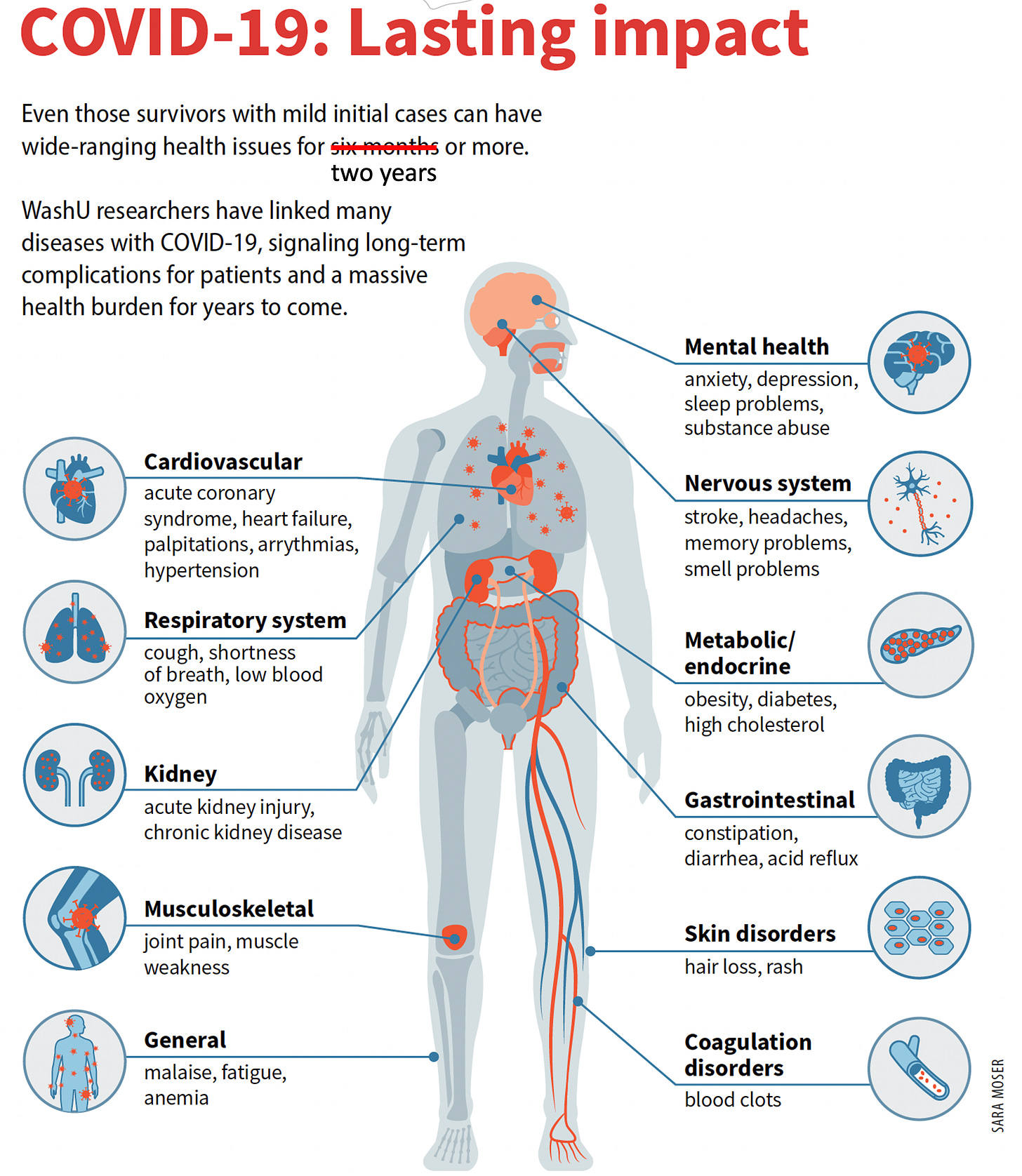
Here is the complicated graphic for all 80 sequelae partitioned by non-hospitalized (top for each cell) and hospitalized (bottom for each cell). Gray shading indicates not statistically significant. As you’ll clearly see, there is considerable variability and range for the severity of these features.
The top 2 outcomes, death and (repeat) hospitalization, remained statistically significantly elevated for the hospitalized group, 1.29 and 2.57-fold, respectively.
To the question posed begged by the title of this edition—“how long?”—the only reassuring finding for non-hospitalized people in the study is that many of the 80 sequelae became not statistically significant at 2 years, even though substantial risk remained across multiple major organ systems. We know some people, albeit a small proportion, completely recover over time. One other positive note was the lack of emergence of risk of new sequelae not seen or noted before, such as cancer.
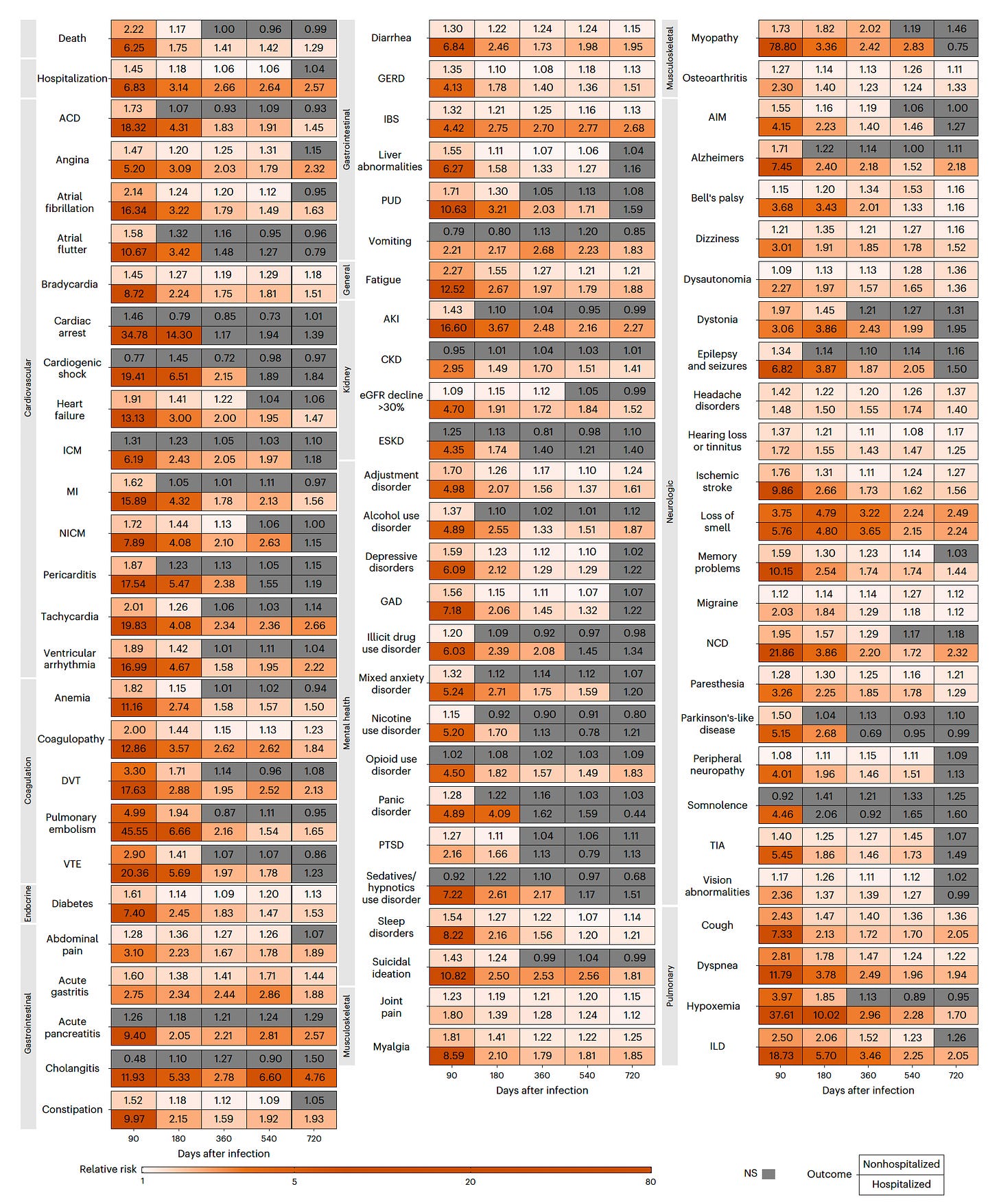
I’d like to point out the data analyzed in this study was enormous, as I tried to capture with one of the supplemental tables below, representative of many others. The authors took on many advanced analytic approaches with weighting, conditional modeling, and sensitivity analyses that I’m not going to review here.
While this is the first comprehensive and systematic study of Covid at 2 years, it unfortunately is within a highly skewed population. The demographics of nearly 90% men, with a mean age of 61 years, is far different than the prototypic person with Long Covid who is more apt to be female and age 30-39 years. Furthermore, to get 2 year follow-up it meant studying a population who had Covid early in the pandemic, before vaccines or the marked evolution of the virus with new variants, including Delta, which was more virulent than the ancestral or Alpha strains that preceded it. So please keep this in mind—the results are important but they may well not be representative of the real world, broader population, of Covid and Long Covid. That’s already a major hole in our knowledge base since there is no other report yet to systematically address a more representative population.
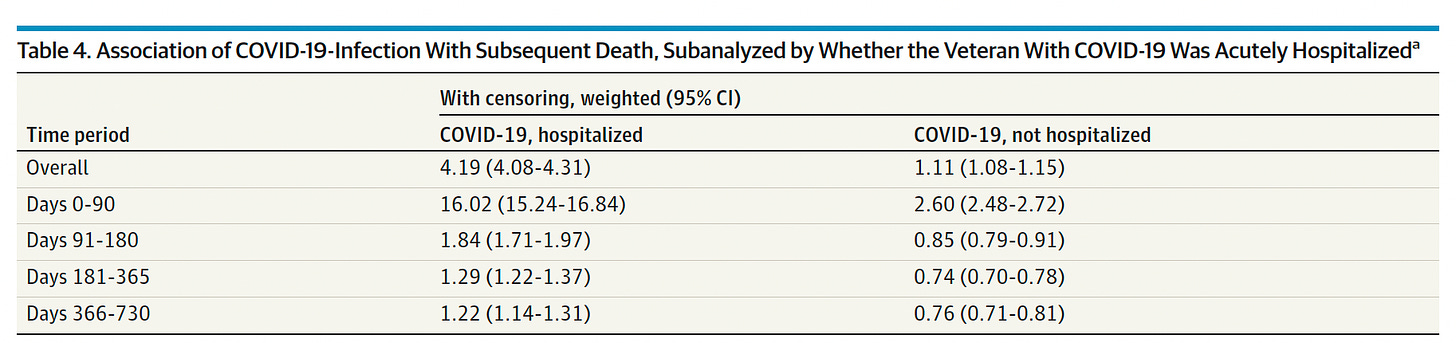
The 2-Year Covid Mortality Report
In JAMA Internal Medicine today, Theodore Iwashyna and colleagues report on over 208,000 veterans with Covid who were compared to matched uninfected individuals for multiple demographic features (age, gender, race, ethnicity, residence and smoking status). Overall, the mortality was 8.7% among the Veterans who had Covid which was more than double that of the non-infected who had a 4.1% death rate. Notably, the hazard of death was concentrated in the first 6 months, without evidence of excess for late mortality. Indeed, the risk of death was 8% less in the Covid Veterans from day 181-365, and 11% less from days 366 to 730 of follow-up. This can be ascribed to the opposite of survival of the fittest, or what has been called “depletion of the susceptible,” a term that I don’t like. But you get the meaning, that the highest risk patients with Covid suffered deaths during the early time period. Of note, and highly consistent with the first study, is the persistent risk of death among the hospitalized, including the magnitude of risk, 1.22 here and 1.29 in the other report. The lack of persistent risk of late mortality (and reduction) is seen only in the non-hospitalized group. Again, let me emphasize that this population is not representative of who were infected with SARS-CoV-2.
Other 2-Year Covid Studies
There are at least 8 that I’ve reviewed and summarized in the Table below; 5 were cited in the Nature Medicine paper. Four of the reports are from China; most are for people who were hospitalized with Covid. Little information is available by organ system. Most had controls groups, some with matching. Overall there was evidence of persistence out to 2 years.
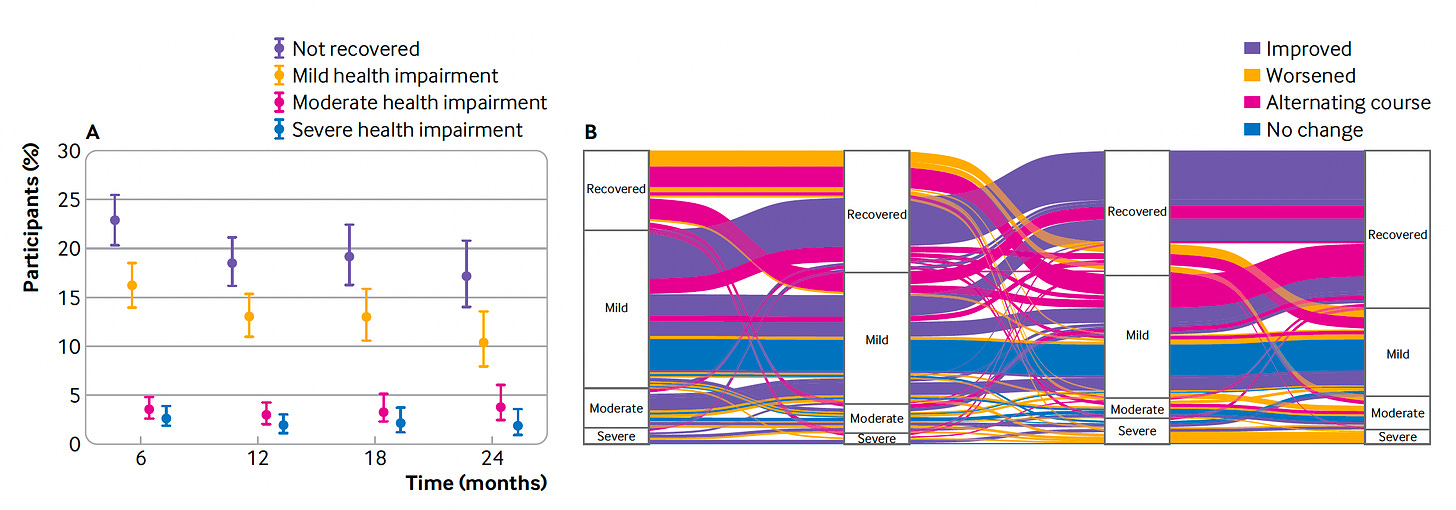
The Ballouz et al paper noted how much the symptoms waxed and waned, some worsening over time, even though the overall trend was improvement.
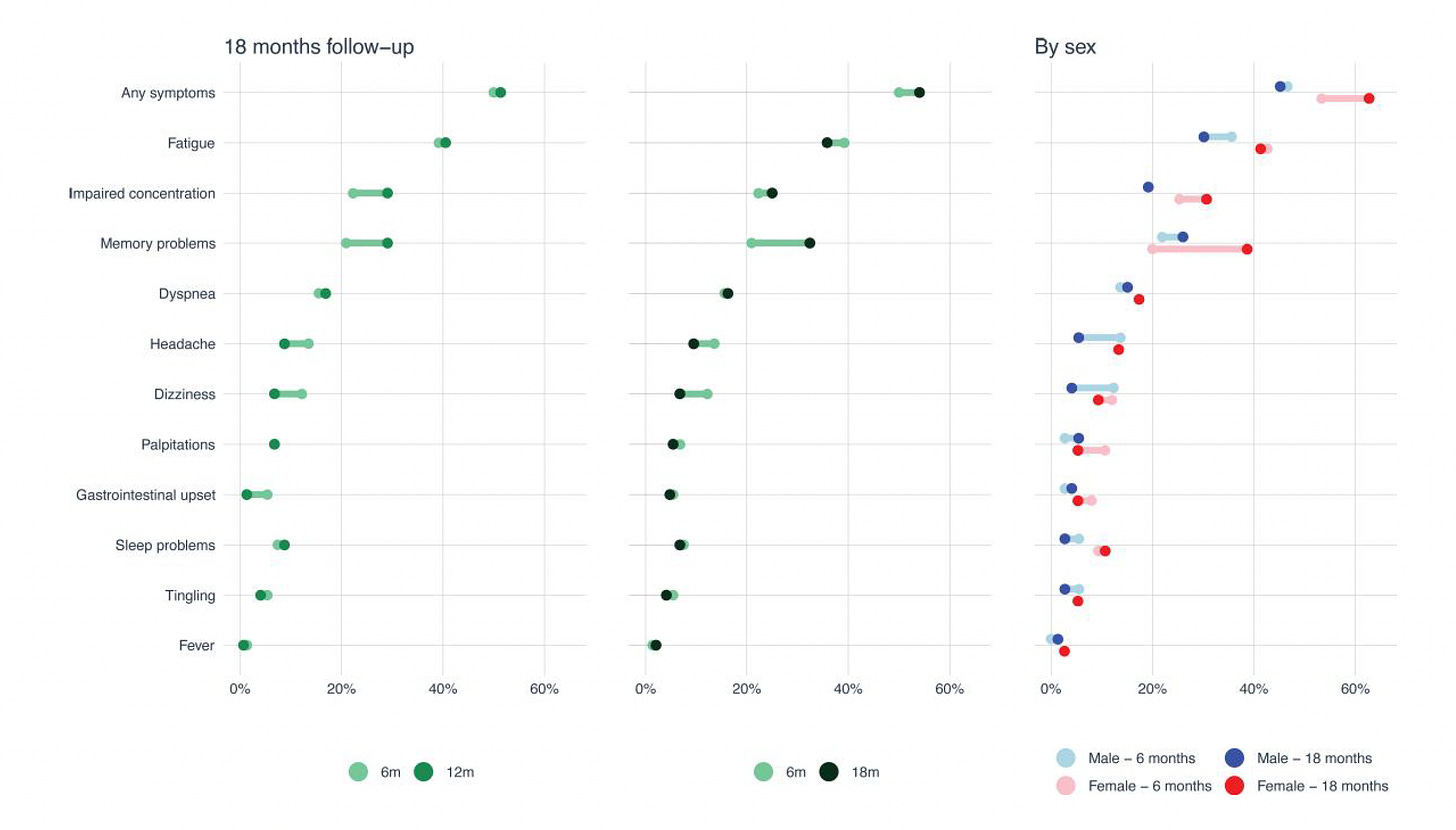
While the Fjellveit report was for a small cohort, these were individuals with mild Covid and the Long Covid symptoms at 18 months differed markedly by gender, underscoring the difficulty of extrapolating from the Veterans cohort.
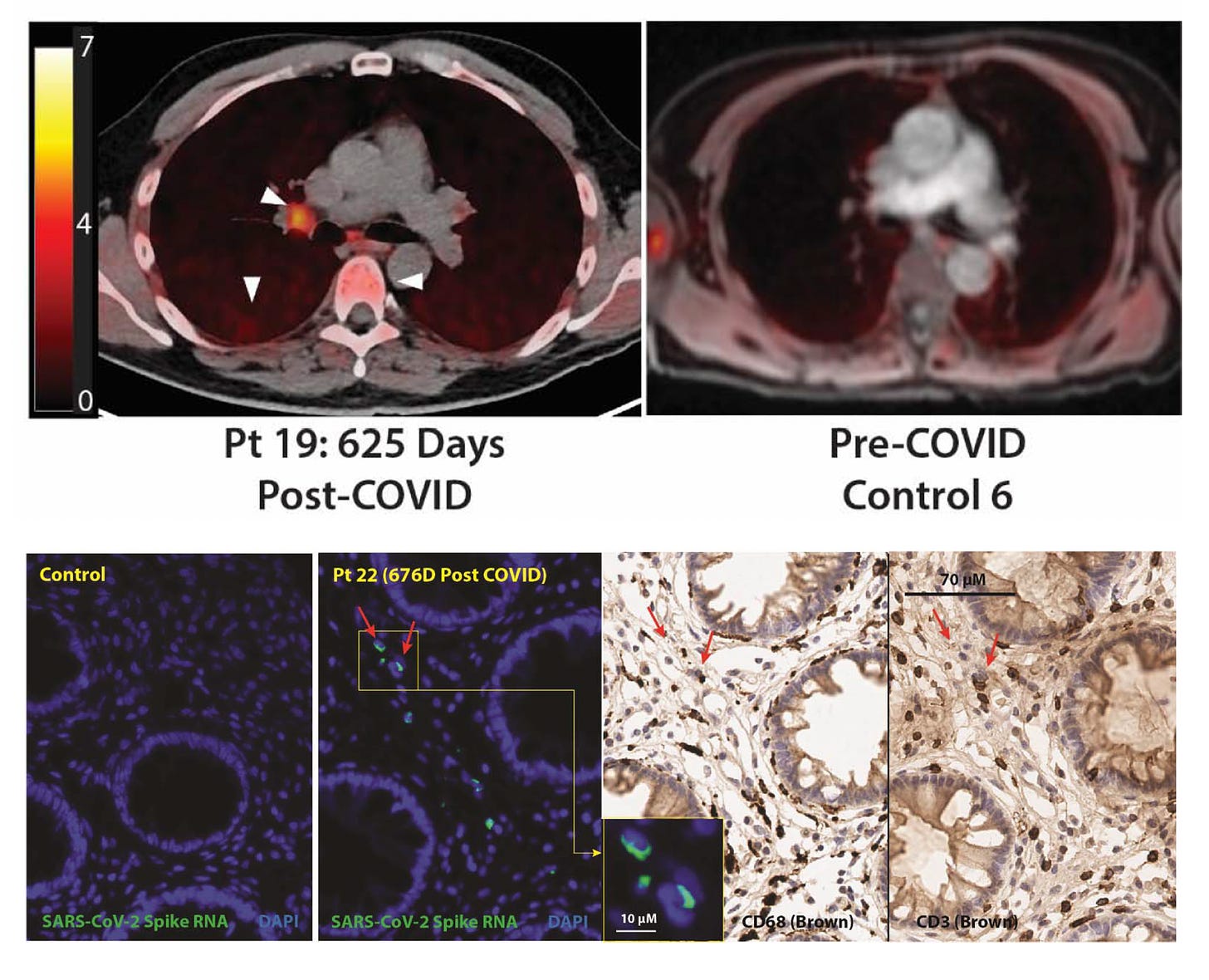
A mechanistic study preprint by UCSF using whole-body PET imaging in 24 participants, out to as long as 910 days post-Covid, provided evidence of persistent T-cell activation in multiple tissues including the brain stem, spinal cord, lymph nodes, cardiopulmonary tissues, and gut wall, which correlated with Long Covid symptoms. Also GI (rectal) biopsy samples showed persistence of the virus—cellular SARS-CoV-2 spike RNA— beyond 2 years in all 5 people assessed.
The Known Unknowns
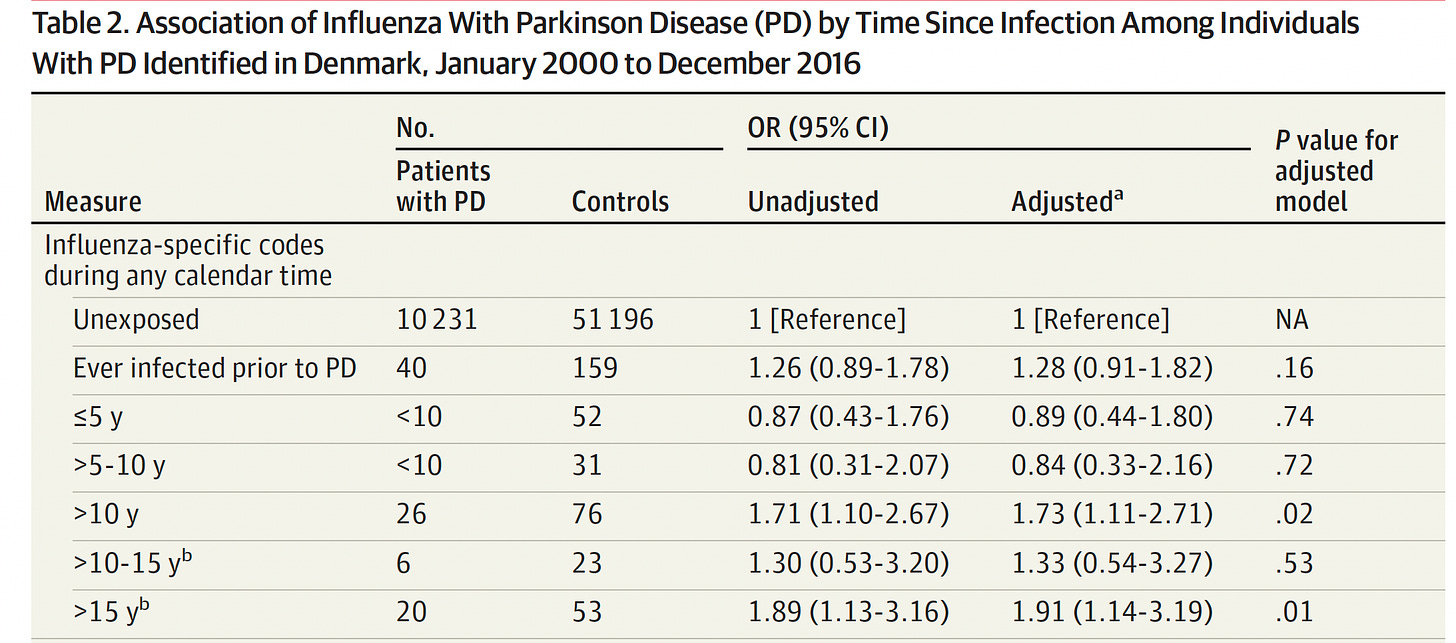
Recall what we’ve learned from previous pandemics—things that are unexpected can be manifest many years later. For example, after the 1918 influenza pandemic, the increased incidence of Parkinson’s disease was noted many years later: “Those who were born between 1888 and 1924 – meaning they were either infants or in young adulthood at the time of the pandemic – appeared to have been 2-3 times more likely to develop Parkinson’s disease at some point in their life than those born at different times.” More recently, in a case-control study from Denmark of over 61,000 individuals, at a decade or longer following influenza infection, a similar relationship was found.
The post-polio syndrome (PPS) was only recognized 15 to 40 years after infection and recovery from polio, with its characteristic muscle weakness and atrophy.
These are just a couple of examples of outcomes not seen in the first 2 years of follow-up after mass exposure to a virus.
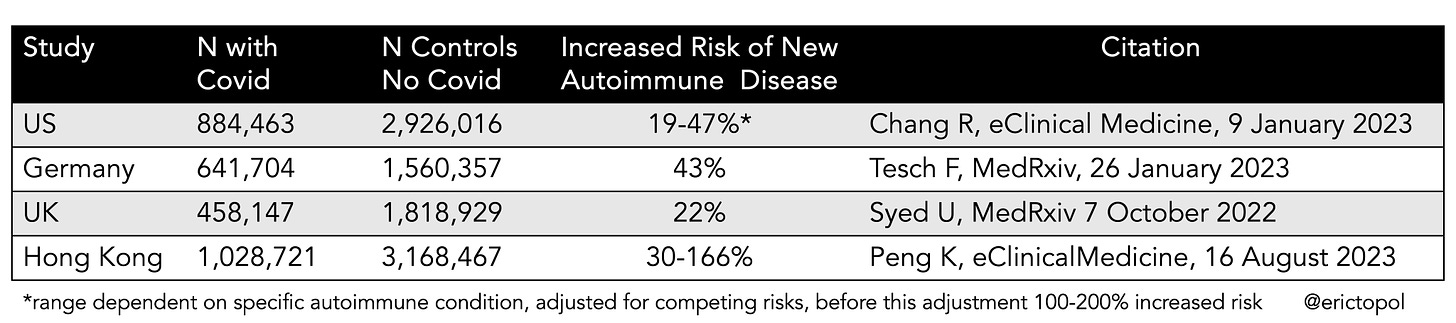
Recently, we have seen the increase in a variety of autoimmune diseases (such as rheumatoid arthritis, multiple sclerosis, Graves’ disease, spondyloarthritis, or psoriasis) in 4 very large cohorts, in 4 different countries, as shown below. There was a consistent increased risk that ranged from ~20 to well over 150%
The most recent one by Peng and colleagues also suggested that vaccines offered protection against manifesting autoimmune diseases. These 4 reports are noteworthy because none of the 2-year studies, including the new Nature Medicine report, assessed the incidence of autoimmune diseases in aggregate. And without including individuals who were vaccinated in studies with extended follow-up, the potential for protection vs sequelae couldn't be seen.
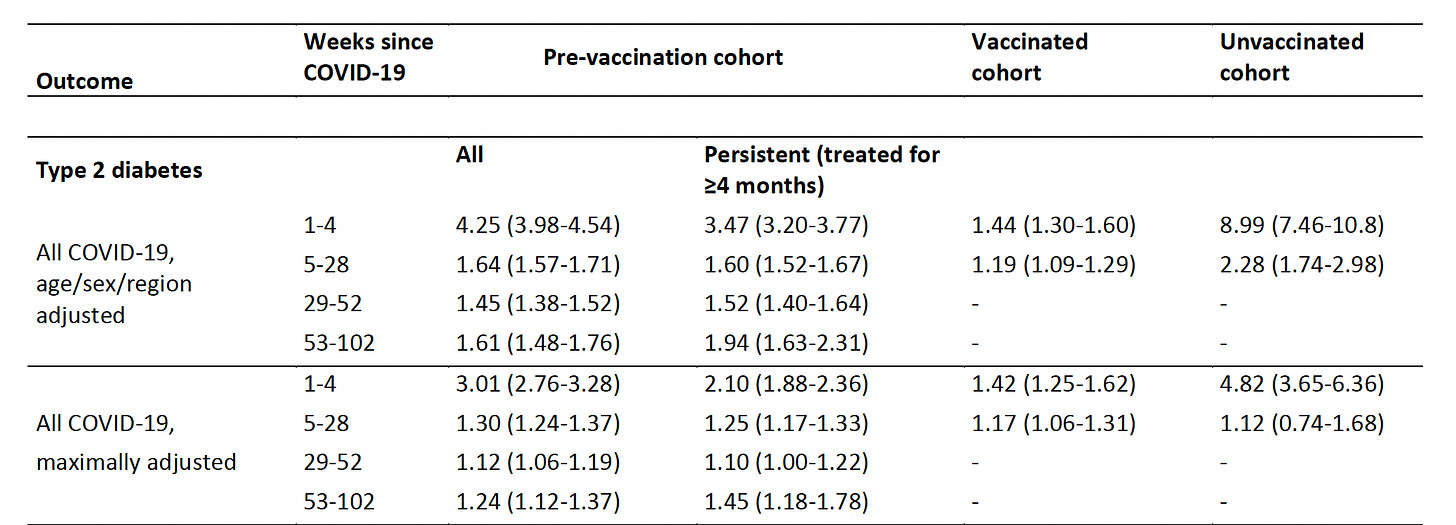
The same applies to diabetes. I previously reviewed the increased risk of both Type 2 (particularly) and also Type 1 diabetes in 14 studies, and what is known about the mechanisms involved. A meta-analysis demonstrated more than 60% increased risk, or at the population level an excess 3 to 5%. A new report was just preprint published earlier this month for diabetes among 15 million people in England. The Table below shows the heightened risk for Type 2 diabetes (the same trends seen with Type 1 but not seen at 1 year). The impact of vaccination for reducing diabetes (vs unvaccinated) was quite substantial.
Why do I bring up diabetes? Because it is an important sequela of Covid, as reported in the new Nature Medicine paper. But the impact of diabetes—the secondary outcomes per se— will not likely be manifest for several years. This represents another category of known unknowns, organ systems that were affected by Covid, including the brain and endocrine, but may on their own drive a wave of adverse outcomes.
That brings me to atherosclerosis. A recent lab study showed SARS-COV-2 viral RNA detectable and capable of replicating in coronary atherosclerotic lesions at autopsy in a small cohort of 8 individuals. Further, atherosclerotic vascular explants were demonstrated to have inflammation induced by SARS-CoV-2 macrophage infection. This report was the first to show the virus in human coronary arteries, but also provides another dimension of unknowns—-the things we are just now discovering. No less, if coronary atherosclerosis is promoted by Covid, that could play out over time with a higher risk of serious events not seen in the acute phase (see Heart attacks late after Covid). Likewise, the compelling demonstration of SARS-CoV-2 spike in the skull bone marrow-meninges and brain at autopsy from people who had Covid, but died of other reasons, raises the concern about brain neuro-inflammation.
Summary
At two years after Covid, there’s a persistent and considerable burden of symptoms and multi-system organ involvement in an important subgroup of people. It’s also unpredictable who will be afflicted with protracted symptoms and new medical diagnoses. While there still is no validated treatment (the Big Miss, as recently reviewed), Long Covid marches on, not just over time for most of those already suffering, but also among newly infected or re-infected individuals —like we are seeing now with increase in cases in the United States and many other countries. The main emphasis here, beyond the enduring and very concerning symptoms and organ dysfunction, is that we are still in the dark. It will take many years to fully know the sequelae of Covid, be it from unforeseen, delayed adverse outcomes like what occurred many years after influenza or polio, or the secondary outcomes of organ systems that are clearly affected, or via promotion of autoimmune conditions or pro-inflammatory pathways, potentially exacerbating risk of atherosclerosis. We’re going to need many more years of careful follow-up to fully understand the ways and extent to which Covid has hurt us. Meanwhile, beyond the known strategies for prevention of infection, we must consider finding effective ways to treat people who suffer from Long Covid as an urgent and foremost priority.
Thanks for reading, sharing and subscribing to Ground Truths!