New Insights into Acute and Long Covid
Four new studies illuminate biologic underpinnings + an update
We’ve been struggling to understand what gets off the track with the immune response in people with Long Covid. Two new reports have shed considerable light on this complexity. Two others inform us about the protection from acute Covid and the importance of vaccination to protect against neurologic sequelae.
Transferring Antibodies from People to Mice
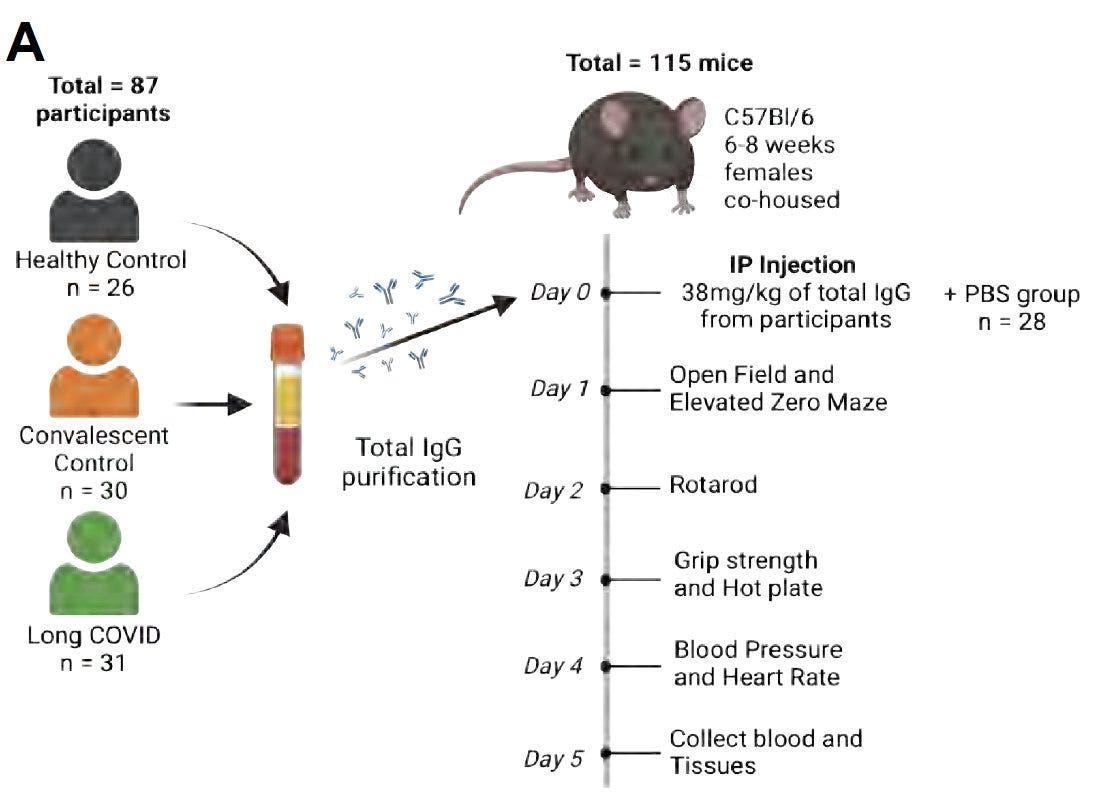
Recently, Jeroen den Dunnen and colleagues at Amsterdam Institute for Infection and Immunity preprint published a study giving IgG antibodies from people with Long Covid (LC) and healthy controls to mice. That induced mice with pronounced hypersensitivity (quicker reaction time) and reduced locomotor activity, related to the proteome profiles of the individuals with LC.
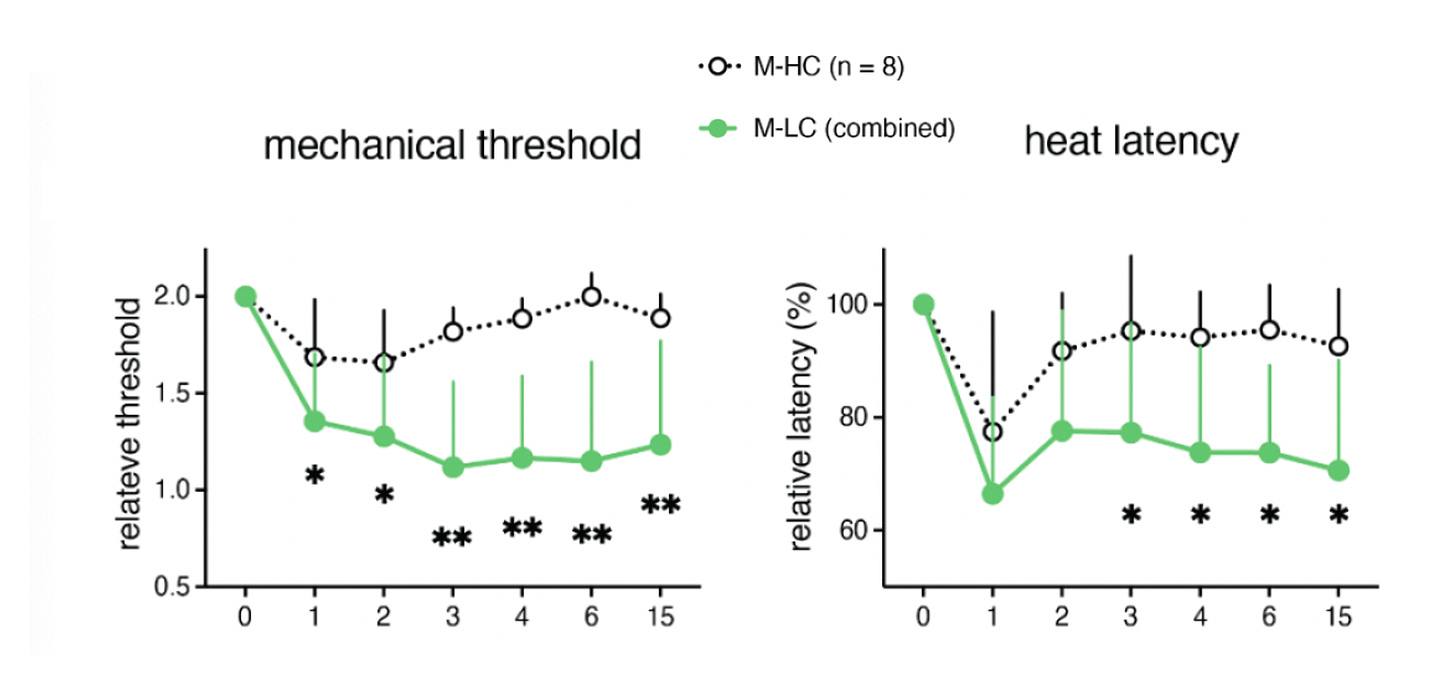
This week a new report from the Iwasaki and Putrino team involving the Mount Sinai-Yale group of LC participants and controls was similar with respect to assessing the antibodies from affected individuals with substantial neurological symptom burden (N=55), people who had recovered from LC (N=42) and uninfected, healthy controls (N=39). The IgG antibodies from the first group were highly reactive to CNS tissue of mice and humans, especially enhanced from individuals with LC who had neurologic symptoms of headache and dizziness. Analysis of the antibodies showed there was a significantly higher auto-antibody proportion in the LC group, particularly CNS-directed.
After transfer of the IgG antibodies to mice there were multiple assessments, as shown below, that yielded some important results.
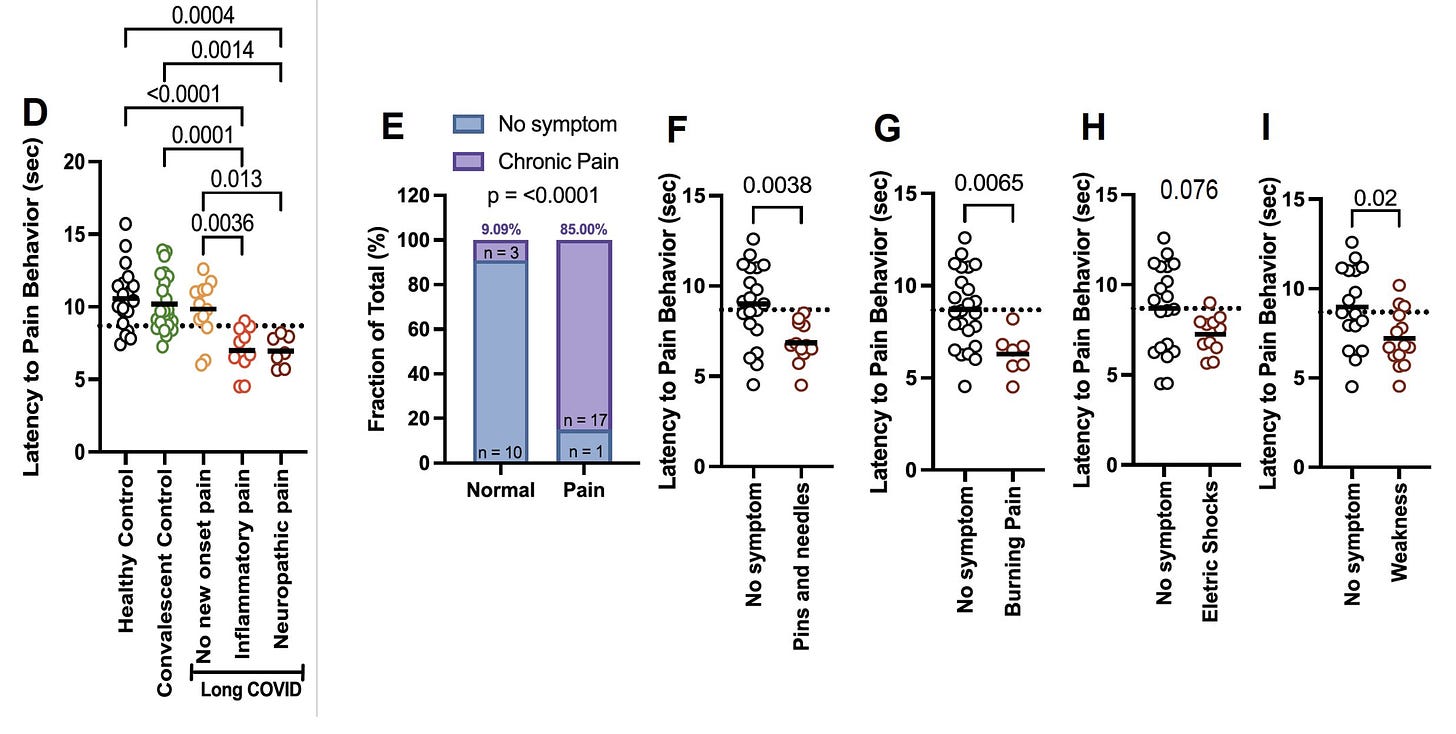
Among the individuals with LC with pain, their IgG injection to mice demonstrated hypersensitivity by shortened latency period to pain (pain phenotype, Panel D) . 85% of the mice with the pain hypersensitivity were concordant (Panel E) with the people with LC who had new-onset pain, as were neuropathic symptoms (Panel F through I) with their diagnosis.
The mice with the pain phenotype were assessed for nerve fibers with findings consistent with small fiber neuropathy, a not uncommon feature in people with LC.
This study not only independently corroborates the Amsterdam report but extends it with a striking alignment of various symptoms in people with the phenotype in mice, in may ways recapitulating the illness. It establishes causality of self-directed antibodies in Long Covid.
That doesn’t negate the potential role of persistent virus/virus remnants or reservoir, or other biologic basis of LC the could serve as triggers, but tells us that the antibodies are functional and playing an important part in the underlying biology of Long Covid.
Immunologic Protection from Getting Covid
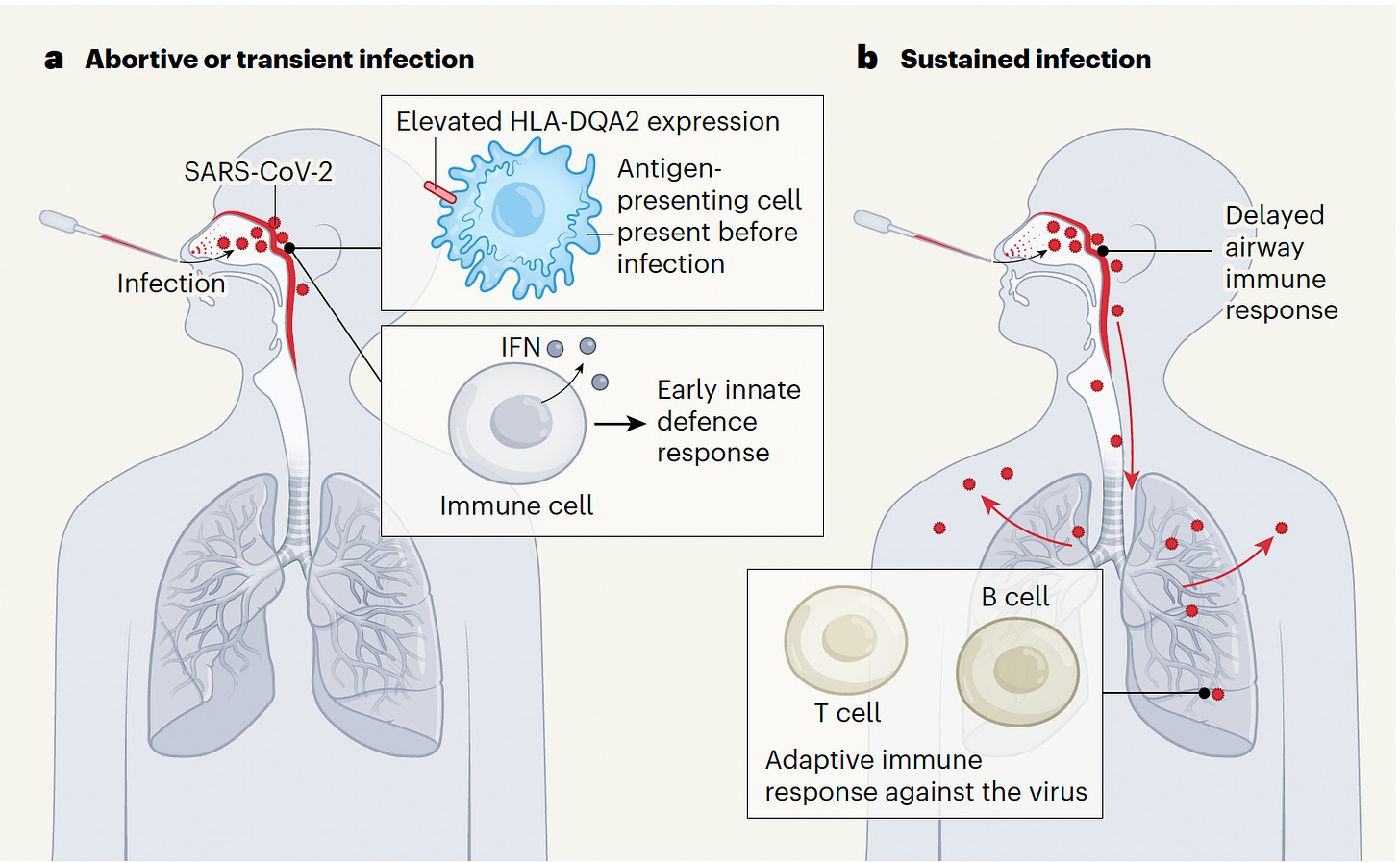
This week in Nature, Rik Lindeboom and colleagues from the Wellcome Sanger Institute reported results from a SARS-CoV-2 ancestral strain challenge study in young, healthy participants who had not been previously exposed. The team did extensive assessment of the immunologic basis (innate and adaptive) and for why participants aborted infections or only showed very transient, minimal response as compared with those who had mild, acute Covid.
The main findings were summarized by Benjamin Israelow and Akiko Iwasaki in an accompanying Nature News and Views with the graphic below.
There appeared to be 2 explanations for the protection from a sustained infection, Either a heightened early Interferon-1 (IFN-1) response of the innate immune response or higher levels of mRNA that encodes for the HLA-DQA2 protein , reflecting elevated expression of this protein on the surface of cells present before exposure to the virus (we actually don't know if this molecule is expressed on the cell surface. There is a lot of controversy around this). The importance of early IFN-1 in the response to the virus has been seen in prior studies and supports the potential role of IFN-1 early intervention to prevent Covid.
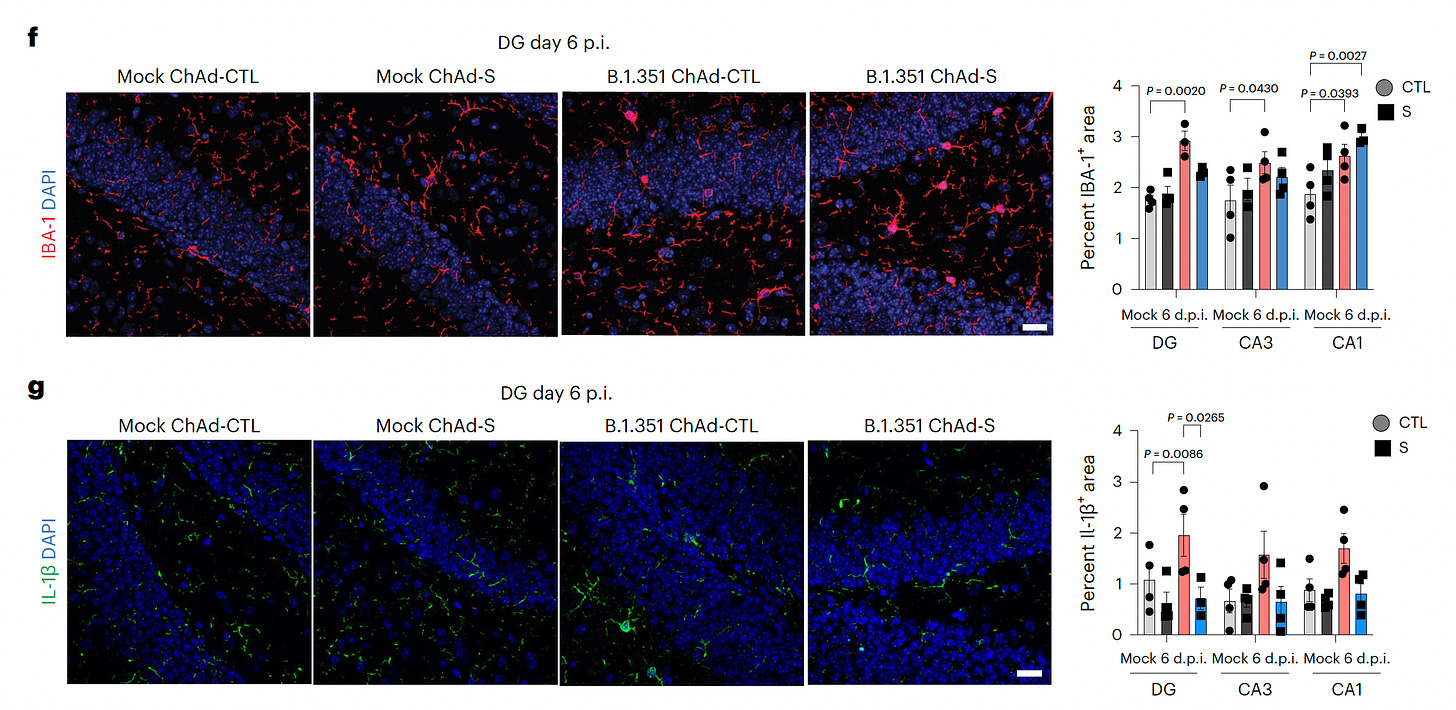
Vaccine Protection from Brain Involvement of Covid (Mouse Model)
In a study by Robyn Klein and colleagues at Washington University St. Louis, mice were given the SARS-CoV-2 Beta variant. That demonstrated brain microglial activation, accumulation of Interleukin-1β, loss of hippocampal neurogenesis, and memory deficits. That was not seen with influenza infection. When an adenovirus vaccine was given before infection, the memory deficits and loss of hippocampal neurogenesis, and interleukin-1β production were limited.
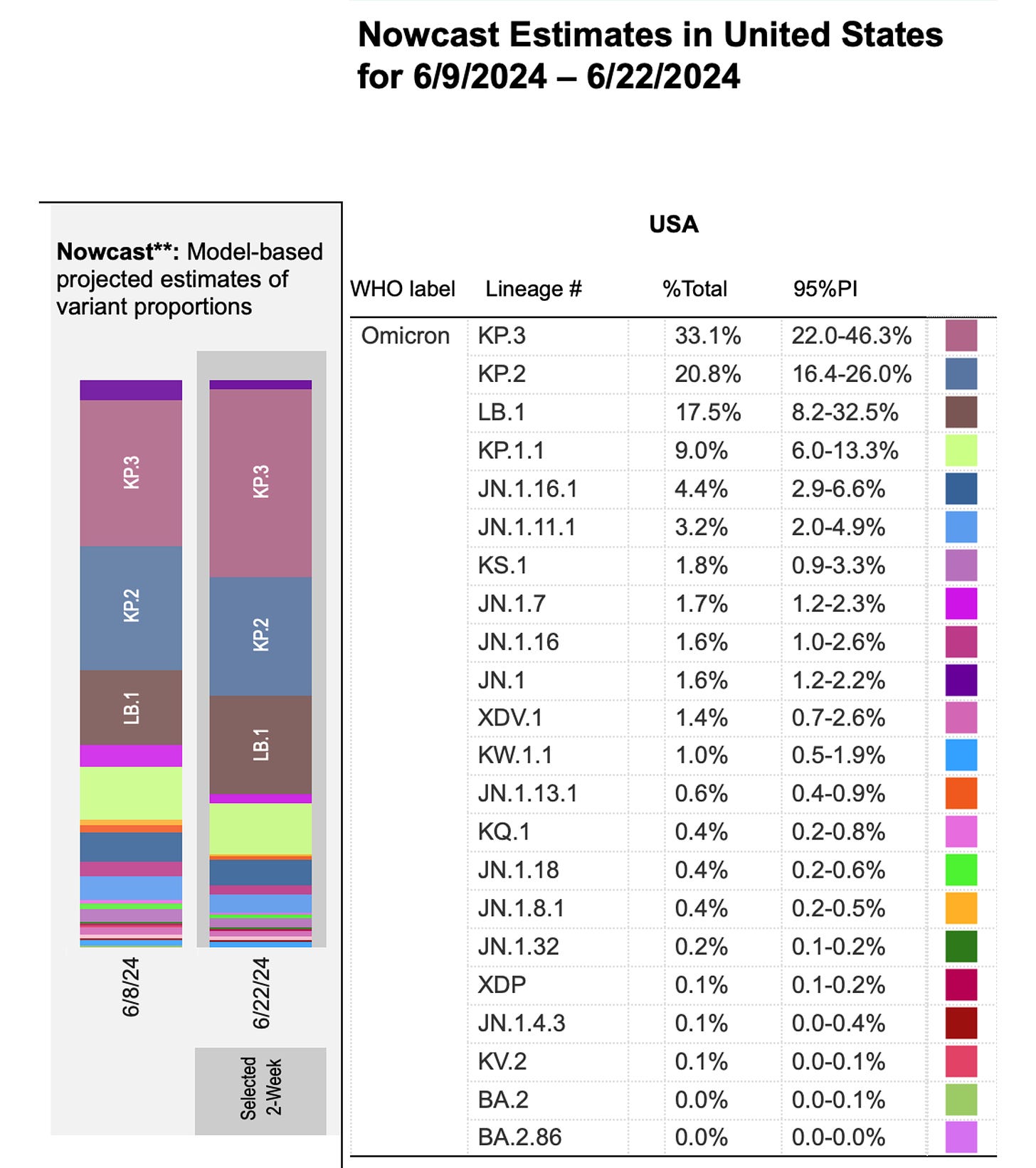
Update on Covid
The CDC released updated data to show some further rise of the KP.3 variant, now accounting for 1 of 3 new cases. The JN.1 variant is fading away.
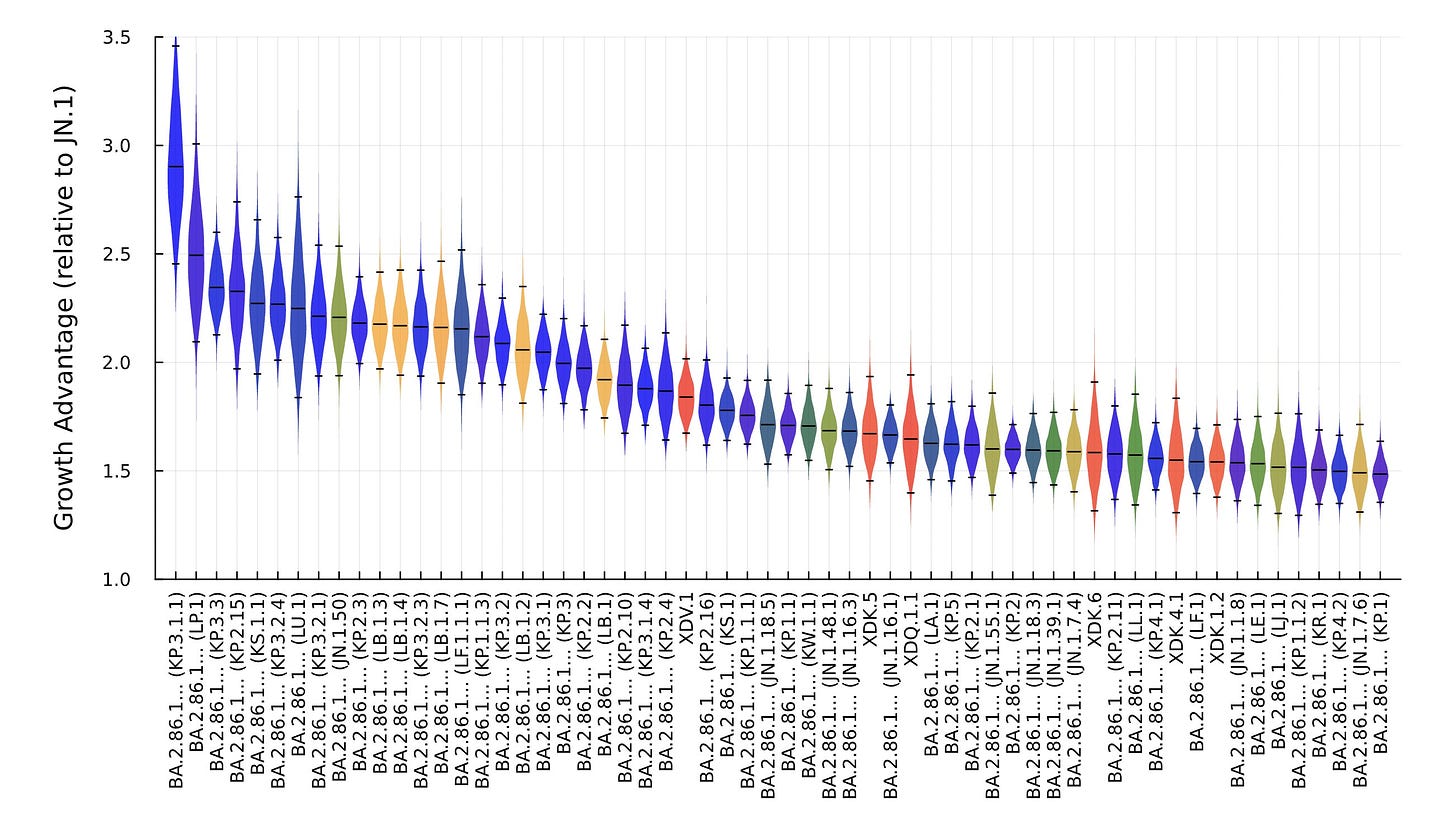
This graph by Ben Murrell shows why this occurring, with KP.3 having a distinct growth advantage compared with all of the other circulating variants.
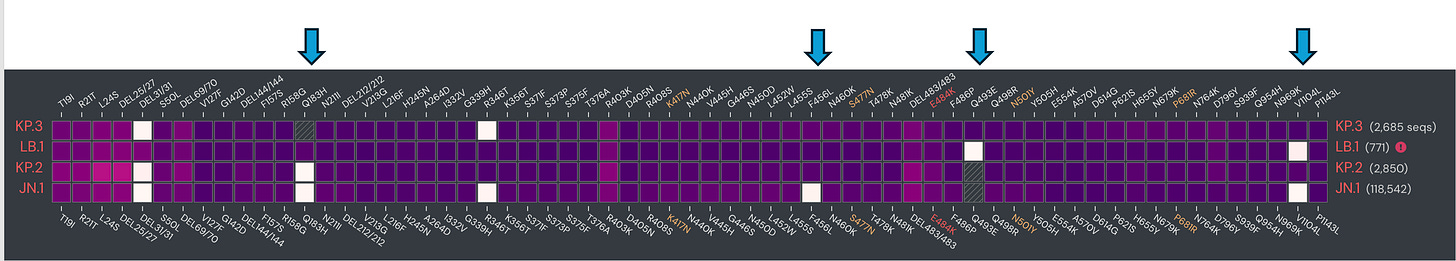
Here are the mutations in the KP.3 spike compared with other variants that are playing a role in its growth advantage.
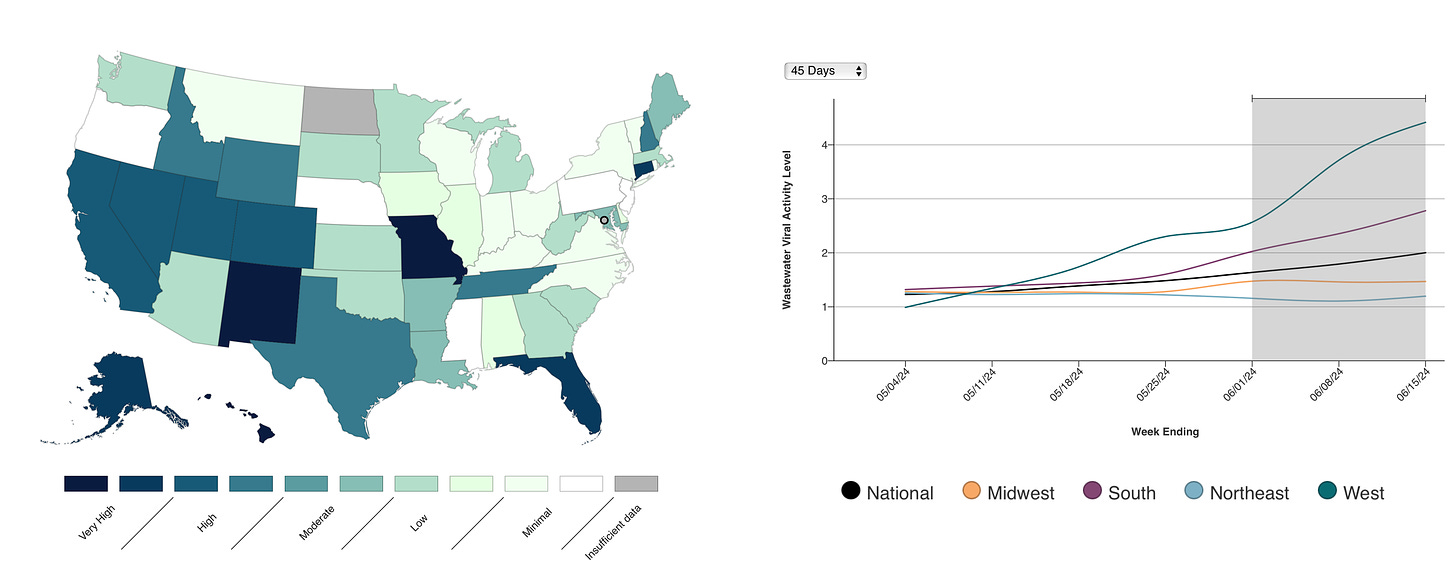
Wastewater levels are on the way up, especially in the West region, from the CDC June 20th update.
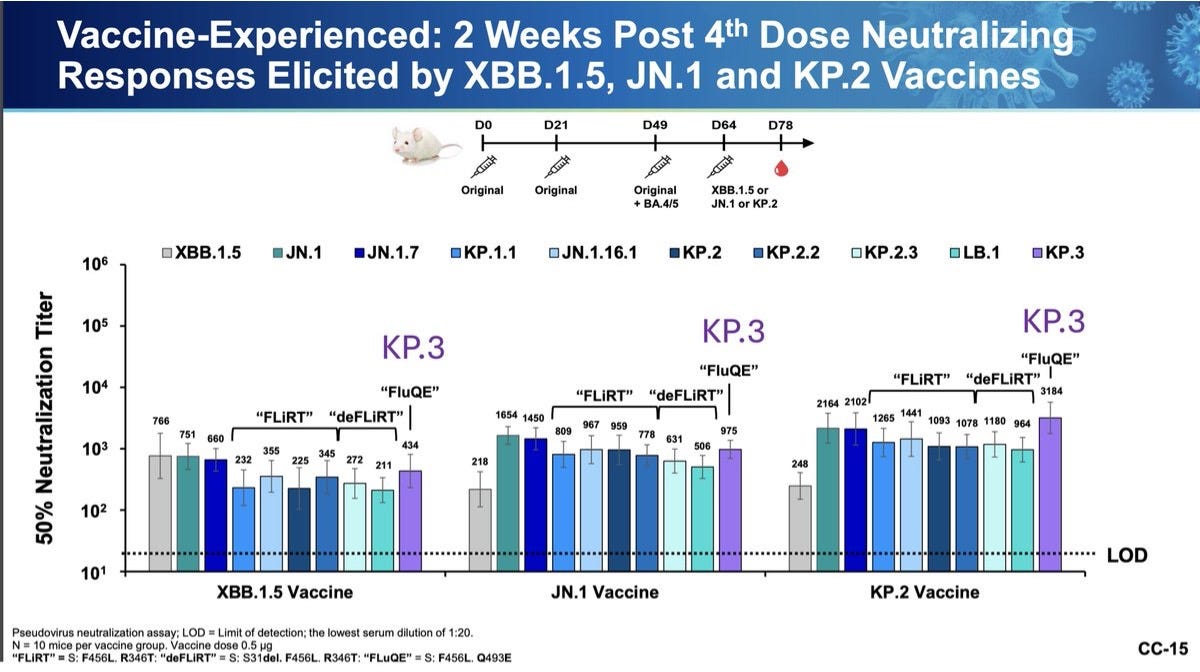
KP.3’s rise is linked to trouble in multiple countries in Europe and Australasia. It’s a good thing that at the last minute the FDA decided to go ahead with the KP.2 vaccine booster for September instead of JN.1 that was the plan from the advisory committee. The neutralizing antibody levels induced by the KP.2 booster were more than 3-fold increased compared to that induced by a JN.1 booster. The plan is that Moderna and Pfizer will have a KP.2 booster ready, and Novavax will go with JN.1
Summing Up
SARS-CoV-2 is still evolving, and by selection will continue to find ways to induce (re-)infections despite global complacency. We’re making progress in elucidating the genesis of Long Covid, with a pair of studies that incriminate autoimmunity as a culprit. At the same time, we’re learning about ways to protect from infection (particularly IFN-1) and how to reduce the chances of central nervous system involvement by vaccination. These are all important steps of progress.
***********************************************
The Ground Truths newsletters and podcasts are all free, open-access, without ads.
Please share this post with your friends and network if you found it informative
Voluntary paid subscriptions all go to support Scripps Research. Many thanks for that—they greatly helped fund our summer internship programs for 2023 and 2024.
Note: you can select preferences to receive emails about newsletters, podcasts, or all I don’t want to bother you with an email for content that you’re not interested in.



Thank you for the update, and good to see some progress in understanding LC. I was also relieved to learn that “at the last minute the FDA decided to go ahead with the KP.2 vaccine booster for September instead of JN.1 that was the plan from the advisory committee. The neutralizing antibody levels induced by the KP.2 booster were more than 3-fold increased compared to that induced by a JN.1 booster. The plan is that Moderna and Pfizer will have a KP.2 booster ready, and Novavax will go with JN.1.” I feared, from reading Katelyn Jetelina’s excellent report on the advisory meeting, that they would go with JN.1 to avoid confusion. I tend to think it’s always a mistake to make decisions like this based on concern about confusion; instead, that should be dealt with separately, as a public communications issue.
Also, just a silly side note: I was in San Diego last week visiting my almost 96 year old mom, and at one point we passed by Scripps. So of course I reminded her that’s where you work, and about all the good information you’ve put forth—and continue to put forth—about Covid (and so many other things). I truly don’t know how you read, grasp, and synthesize so much complicated information at what appears to be lightening speed! Even though a good bit of the detail is often above my pay grade, I am endlessly appreciative, and Mom was impressed too!
Should we be screening blood donations for long covid if it is easily transferred to mice?