Our Body Axis Maps Are Getting Redrawn
New circuits discovered, old ones refined
We’ve long known about the intra-body connection like the brain-heart axis, the explanation, among other conditions, for the “broken heart syndrome” (Takotsubo cardiomyopathy) after an intense emotional or stressful situation. But in just the past week or so there has been a cluster of reports about new body axes or expanding knowledge on ones known to exist. This Ground Truths edition is a roundup of several new reports that in aggregate are illuminating the intricate circuits in our body. Fascinating stuff!
The Body-Brain Axis for the Immune System
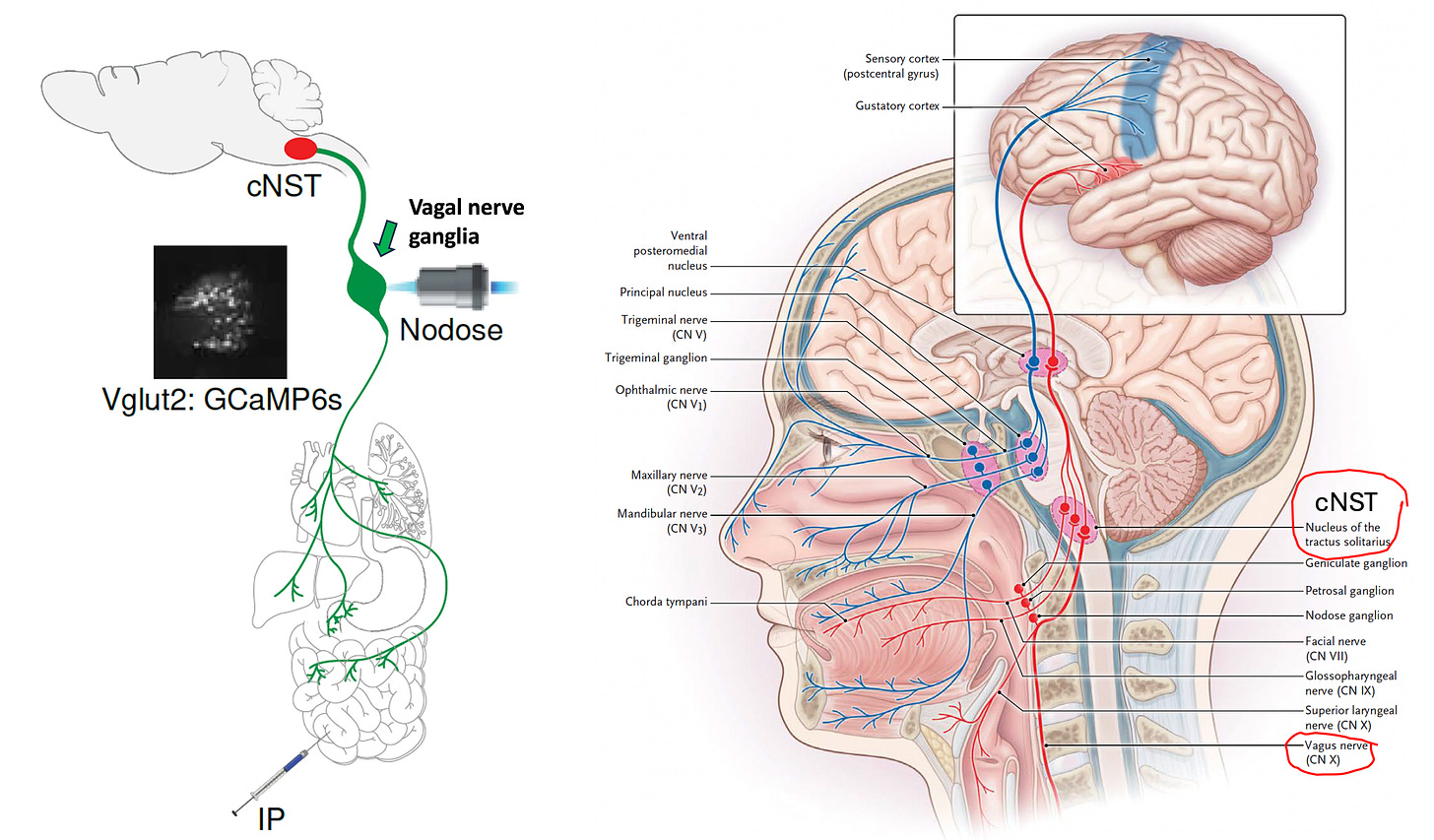
In a Nature paper, Columbia University researchers unraveled the circuit for how immune activation in the body activates the brain. By injecting bacteria compounds into the abdomen (intra-peritoneal, I.P.) of mice that elicited inflammation and an immune response, a region in the brainstem was switched on, as seen by imaging.
The circuit involved the vagus nerve to the caudate nucleus solitaris (cNST) in the brainstem. When the neurons were activated, inflammation was reduced (by ~70%). In contrast, when the neurons were silenced, the immune response was unleashed, and there was a 3 to 10-fold increase in mediators (interleukin-6, IL-1beta, IL-10) of inflammation. There was reciprocity in the circuits with surveillance by cNST/vagal of inflammation signals in the body. That’s akin to a rheostat, a master dial function of the immune system. It’s even more refined than that. By single-cell sequencing it was found there are 2 discrete circuits within the vagus nerve which are divided for response to pro-inflammatory and anti-inflammatory molecules. In the ulcerative colitis (an autoimmune condition) mouse model, the same manipulations of the circuit led to inducing dramatic colitis or protection from inflammation.
As the authors asserted, “Most unexpectedly, this body-brain circuit modulates not only pro-inflammatory but also the anti-inflammatory response.” Accordingly, It’s been called a “black swan event” since the biologic circuitry details were not anticipated. The implications for defining this neuro-immune axis for immune balance are potentially important for better approaches to autoimmune diseases, Long Covid, and dysregulated immune system conditions.
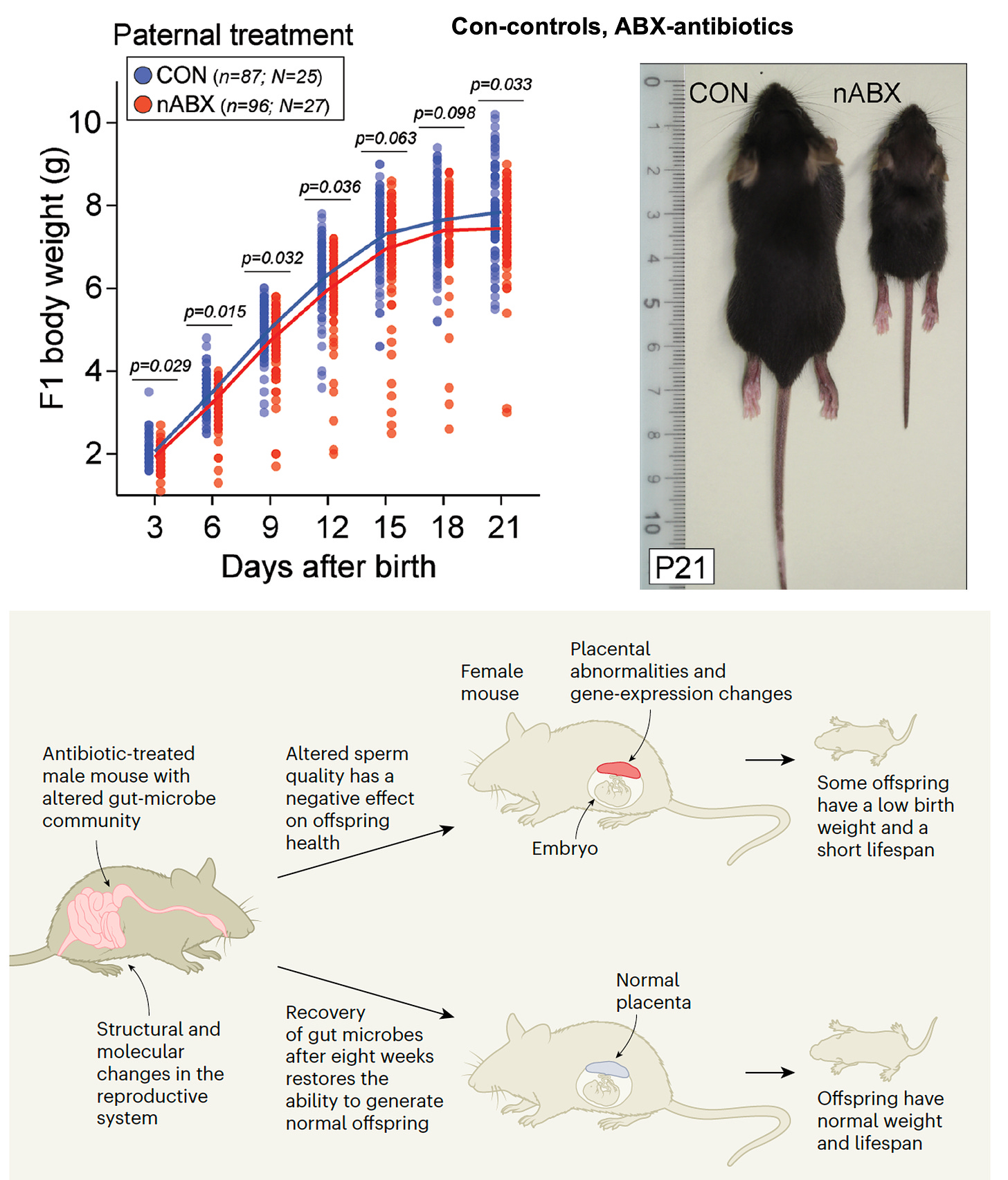
Gut to Sperm Axis
While we fully appreciate the ability to transmit our genome from one generation to another, this had not been expected to occur for our gut microbiome. A European Molecular Biology Laboratory (EMBL) group, led by Jamie Hackett, published evidence in Nature that various perturbations of the gut microbiome in male mice, including antibiotics, diet and laxatives, talk to sperm, with disruption of the microbiome of the testes and male reproductive system, and changes in sperm RNA. This was consequential for the father’s offspring with some mice exhibiting low birthweight and shortened lifespan (Figure below, bottom from accompanying Nature News and Views). Additional experiments showed that restoration of the paternal gut microbiome reversed the effects. Use of IVF and microbiome transplantation indicated this effect was mediated through sperm cells, not via the paternal microbiome. We don’t know if these effects occur in humans, but the implications are big and represent another black swan.
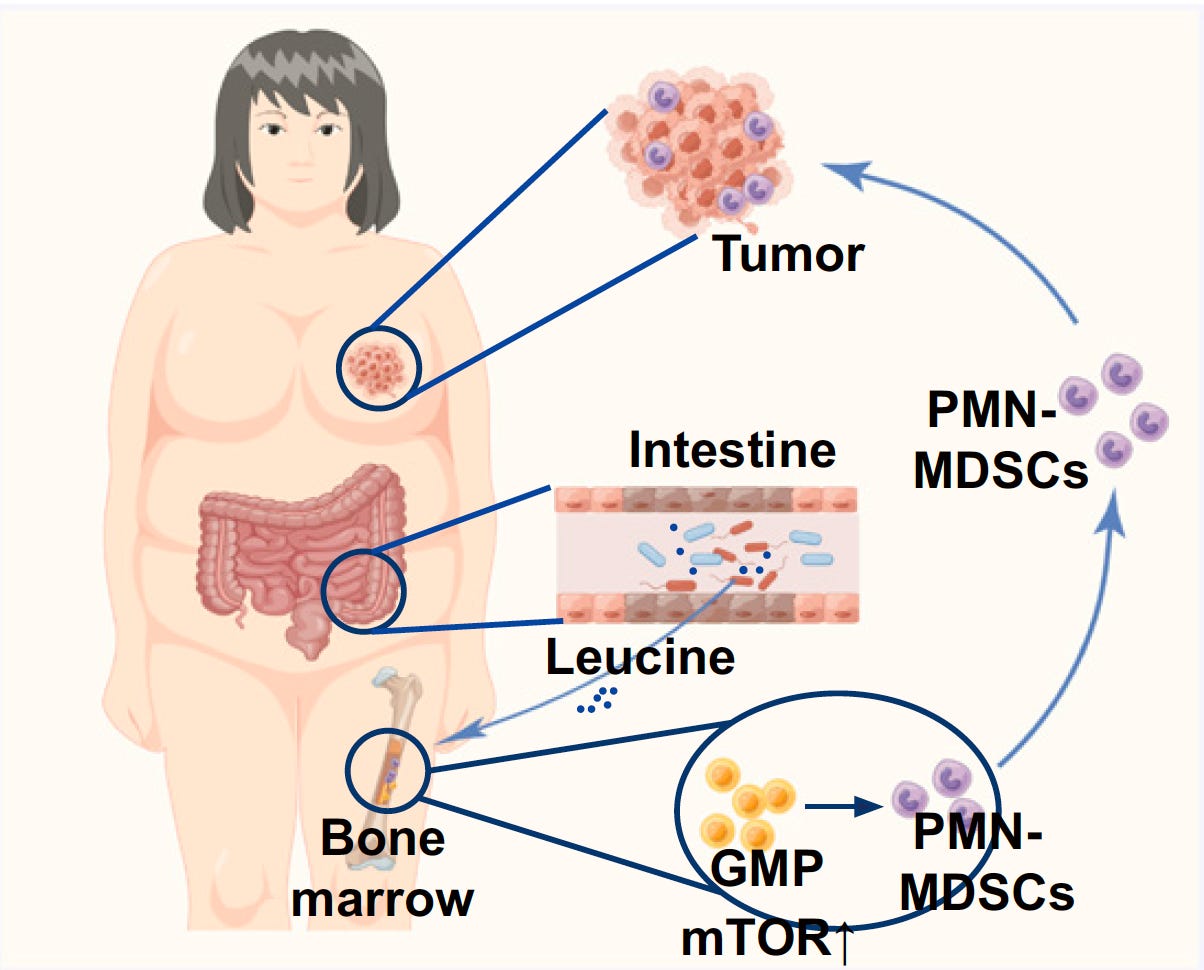
Gut-Bone Marrow-Tumor Axis
The mechanism by which a high-fat diet promotes spread of cancer was worked out in a new paper in PNAS. The high fat diet in mice led to increased leucine production from gut microbiome (particularly linked to a species, Desulfovibrio), activating the mTOR pathway and differentiation of bone marrow suppressor white blood cells (PMN-polymorphonuclear), with tumor progression.
While much of this work was performed in mouse models, some of it was corroborated in patients with breast cancer, such as fecal leucine and white cell differentiation.
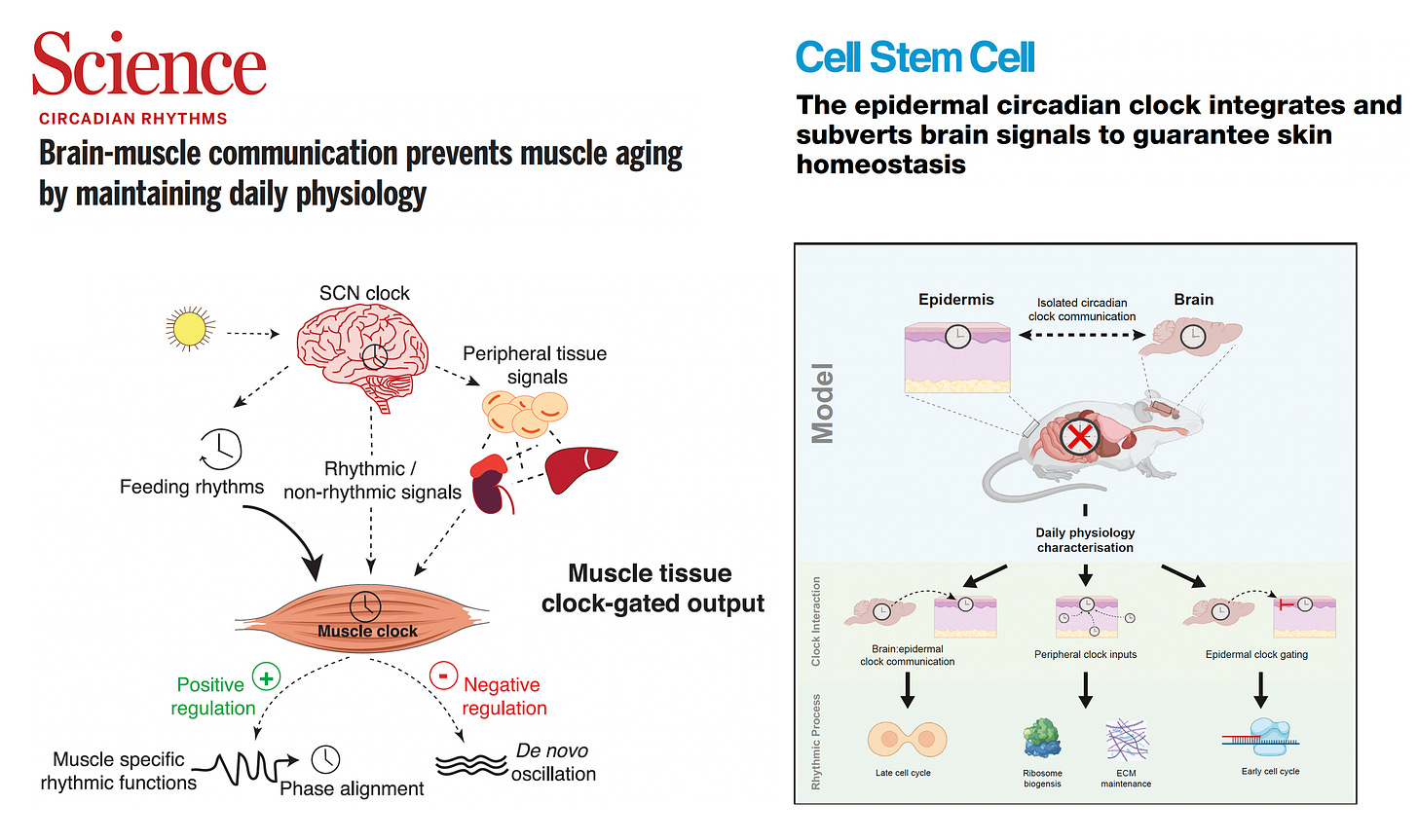
Brain-Muscle and Brain-Skin Circadian Circuits
A pair of papers in Science and Cell Stem Cell by a collaborative research group in Barcelona using the same model, and spotlighting the critical communicative modules of brain to muscle and brain to skin, respectively. Nearly all cells in our body have circadian clocks, but the central clock in the brain—the suprachiasmatic nucleus (SCN)—serves as mission control. But what was surprising was a peripheral (muscle or skin) gatekeeping role of these clocks. The SCN brain clock’s activity and output deteriorate with age. In old mice, time restricted eating helped restore the central clock function and mitigated the muscle mass and strength loss.
For the skin module, the unexpected finding was that the skin circadian clock also relied on other tissues besides the brain SCN, and that the skin clock could not only integrate but also subvert the brain clock. But for avoidance of aging (muscle or skin), the synchronization of the brain and peripheral tissue clocks was important.
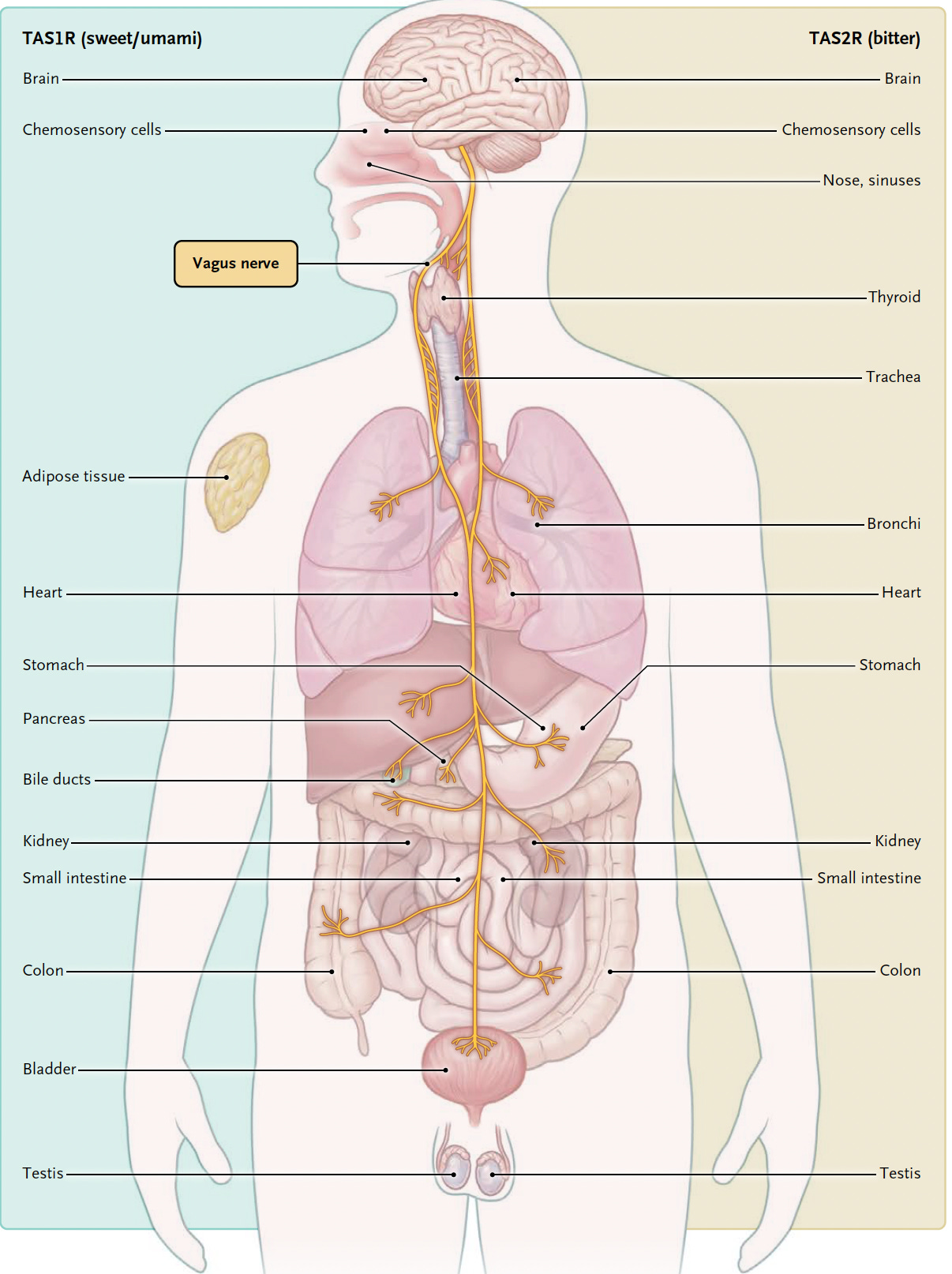
The Vagus Nerve
In an outstanding review of taste and metabolism this week in NEJM the role of the vagus nerve was emphasized. The vagus nerve rapidly (in milliseconds) conveys sugar-sensing information to the brain, and tracks into the brain for the circuitry of reward and appetitive neurons and the hypothalamus. A recent preprint highlighted the gut-brain vagal axis role in mice for hippocampal structure and function, affecting long-term and short-term memory. Previous studies in experimental models indicate the vagus nerve also impacts neuro-inflammation in the hippocampus and other brain regions.
Those of you who listened or read my recent podcast with Dan Drucker will recall that GLP-1 peptides don’t cross the blood-brain barrier but appear to have pronounced effects on brain inflammation, invoking the gut-to-brain axis. More on GLP-1 in the mouse model appeared in a new preprint, with the use of exenatide (an early GLP-1 much weaker than the drugs in current use) given at low dose, below the amount needed to reduce appetite of lose weight. This yielded, in old mice, multi-omic benefit of slowing the aging process biomarkers of DNA methylation, RNA, and metabolites, pronounced in the hypothalamus, and comparable to rapamycin by side-by-side testing. Full circle in this “redrawn” circuitry description: so much of this elucidation for the body-brain axis (first circuit reviewed) builds upon pioneering work in the 1990’s by Kevin Tracey, showing that electrical stimulation of the vagus nerve markedly reduces inflammation.
Summary
The use of advanced techniques, including imaging, single-cell sequencing, and optogenetics, are helping us understand our intra-body circuits. Such work is accelerating, as evidenced by this recent crop of impressive reports appearing within a matter of days. It would be easy to conclude that everything is connected to everything, but it’s the granular details of these circuits that will be crucial to know and translate for potential clinical benefit. Who would have anticipated that fathers could transmit gut microbiome signals through their sperm to their offspring (if this holds up in humans)? Or that there’s a master immune rheostat in the brain cNST? No less the vagal nerve’s ever-expanding, pluripotent role. What we’re seeing in just one post, with the circuits delineated to some degree here, has substantial relevance to all major diseases including autoimmune, cancer, neurodegenerative, and even the process of aging. Undoubtedly, such illumination off our intra-body circuitry will eventually help us make critical progress for promoting health and preventing disease.
Your support of subscribing to Ground Truths, and sharing it with your network of friends and colleagues, is much appreciated.
The Ground Truths newsletters and podcasts are all free, open-access, without ads.
Voluntary paid subscriptions all go to support Scripps Research. Many thanks for that—they greatly helped fund our summer internship programs for 2023 and 2024.
Note: you can select preferences to receive emails about newsletters, podcasts, or all I don’t want to bother you with an email for content that you’re not interested in.
Comments for this post are welcome from all subscribers.



Amazing stuff. Clearly what happens in vagus doesn’t stay in vagus…
As a non-medical person, but was able to understand just enough to want a further explanation. Thank you for sharing information such as this with us.