Our Sleep, Brain Aging, and Waste Clearance
How sleep prevents "dirty" brains that age faster
“Sleep is a non-negotiable biological state required for the maintenance of human life.…our need for sleep parallels those for air, food, and water.”—Grandner and Fernandez
Discovery of Glymphatics
In 2012, Maiken Nedergaard and her colleagues at the University of Rochester discovered the brain glymphatic pathway, the brain’s plumbing system similar to lymphatics in the body (but without lymph nodes), which consists of a network of fluid-filled and water channels (specifically aquaporin-4, AQP4, expressed on astrocytes) alongside (para) blood vessels to drain chemical waste, and facilitate movement of cerebrospinal fluid.
Since the initial discovery, we’ve learned much more about how the glymphatic pathway works.
Synchronized Neurons
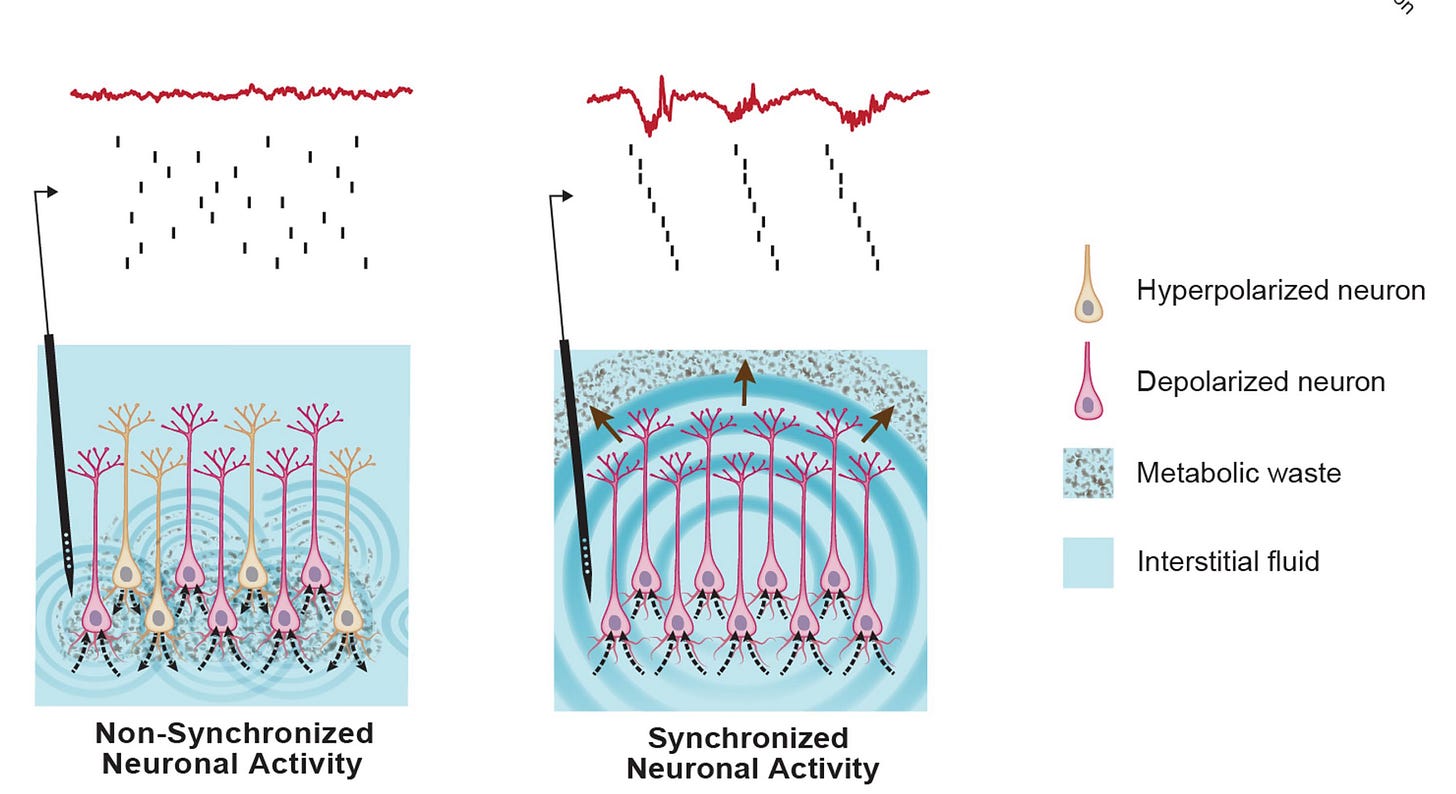
In early 2024, 2 Nature publications demonstrated that synchronized neurons can activate glymphatic waste clearance. Blocking neuronal firing prevented waste clearance (Figure below). The best summary for their work, positioning neurons as the master organizers for brain clearance, as articulated by the authors, is: “neurons that fire together, shower together.” Gamma stimulation was shown to increase the arterial vasomotion (rhythmic oscillation/movement) and release of neuronal peptide molecules.
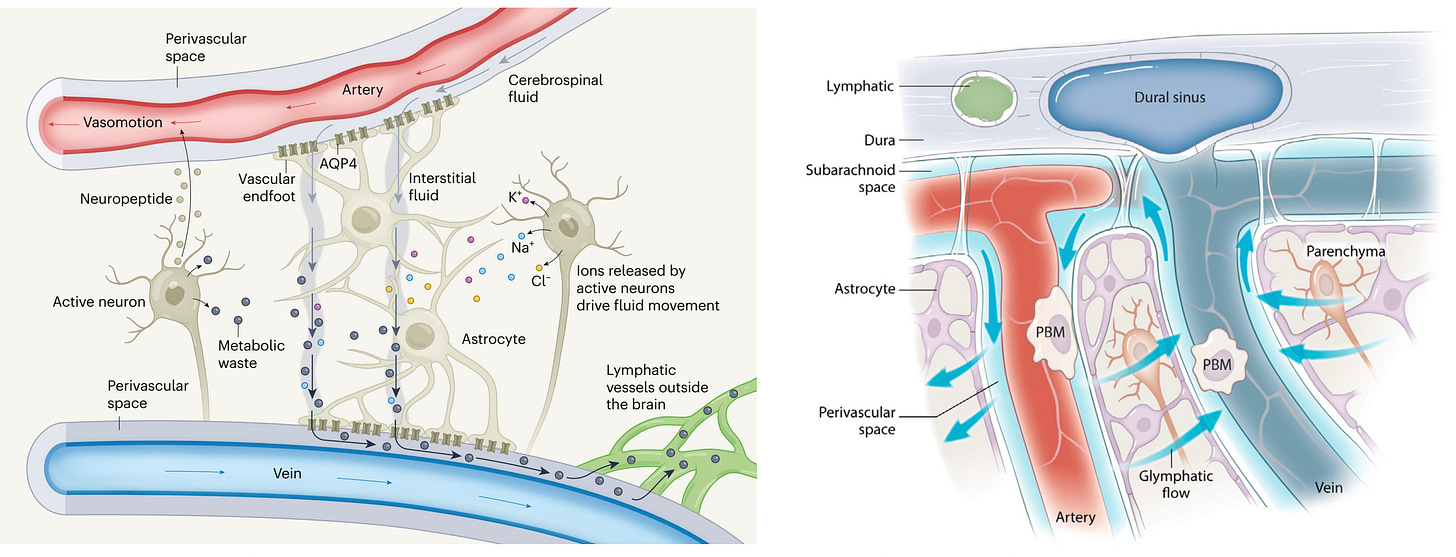
Updating The Glymphatic Mechanisms
The 2 schematics below provide an updated version of our understanding of how glymphatics work. At left, below, you can see key components (neurons, AQP4, neuropeptide, the perivascular space, also known as Virchow-Robin space) with waste material accumulating around the artery (at top), which is subject to vasomotion, and the clearance of the waste material alongside the veins to lymphatics outside the brain (→ meningeal lymphatic vessels and neck lymph nodes). At right, you see the same flow pattern from around arteries to veins to the dural sinus of cerebrospinal fluid. The importance of brain macrophages (parenchymal border macrophages, PBM) is highlighted.
Demonstration in Humans
Until recently, all the work on glymphatics had been done in rodent experimental models. Late in 2024, the first demonstration of glymphatics in humans, among 5 patients undergoing brain surgery with MRI images at two time points, confirmed the presence of this network runing alongside blood vessels in the brain. (The red and white arrows indicate the new appearance of contrast in the 2 sets of paired images below).
The New Study of Glymphatics During Sleep
The pioneer of this field, Maiken Nedergaard, and colleagues, published a new report in Cell this week (main Figure schematic below) . This used “flow fiber photometry,” a new technique—with surgically mounted electrodes with fiberoptic lines for optogenetic tracing— that overrides the problem of previous studies that required anesthesia of mice, and is very different than natural sleep. During non-REM (rapid eye movement) sleep they observed oscillations in the blood brain volume that, with tracing the flow of cerebrospinal fluid, was mediated by norepinepherine levels, serving as a pump. They concluded “we have identified the most important driver of glymphatic flow in non-REM sleep.”
Ambien (zolpidem) was assessed for its effect and it suppressed the norepinephrine effect and reduced glymphatic flow. As a cardiologist experienced with the side-effects of sleep disruption from beta blockers, I wouldn’t be surprised that their inhibitory effect on norepinephrine is the basis for it.
Sleep and Brainwashing
“It’s [Sleep] like turning on the dishwasher before you go to bed and waking up with a clean brain” — Maiken Nedergaard
Sleep is the principal driver of glymphatic flow and waste clearance, occurring during the NREM phase of sleep (which includes deep sleep, slow-wave, known as stage N3). Indeed, the totality of evidence backs sleep’s major function as waste clearance of the brain through glymphatics. Clearance of toxic proteins, like β-amyloid, are critical to brain health. Back in 2018, PET scanning was used to show that one night of sleep deprivation resulted in substantial increase in β-amyloid accumulation, in regions of the brain linked to Alzheimer’s disease. On a chronic basis, several studies have shown that poor sleep is prospectively linked to the risk and progression of Alzheimer’s disease. For example, in nearly 8,000 participants with 25-year follow-up, people aged less than 50 or 60 years with 6 hours of sleep or less had a >20% increased risk of developing late-onset dementia. It’s also notable that clearance of toxic proteins interacts with our brain immune system (as I reviewed in a recent Ground Truths Guardians of the Brain), invoking another mechanism by which waste induces harm.
Brain Aging and Waste Clearance
As we age, efficiency of the glymphatics and vascular dynamics decline (ISF-interstitial fluid) and sleep gets disrupted, there are more arousals, less synchronized neural activity, and less NREM stage 3 deep slow-wave sleep. This week there was a new and outstanding review by Jiang-Xie and colleagues from Washington University, St. Louis in the journal Neuron. As you can see from the schematic below, the aging brain accumulates metabolic waste, with deposition of extracellular matrix (ECM) and progressive dysfunction of the parenchymal border macrophages (PBMs). The all leads to buildup of unwanted, molecular waste in the brain. The accumulation of β-amyloid and tau leads to sleep disturbance and dysregulation or circadian rhythm. Reduced non-REM sleep has been linked to the risk of early Alzheimer’s disease. This appears to be bidirectional, setting up a vicious loop, since decreased sleep leads to more toxic proteins, and the toxic proteins interfere with sleep.
Further, the exit route of meningeal lymphatics is diminished, as shown below, in the aged brain. This is accompanied by an untoward immune response, with expansion of CD4+ and CD8+ T cells, leading to chronic inflammation in the aged meninges which further impairs the exit route of waste from the brain. In experimental models VEGF-C (vascular endothelial growth factor) has rejuvenated these meningeal vessels , which makes this a logical target for preventing age-related decline in waste clerance.
All of these features of impaired waste clearance of the aged brain are especially prominent in neurodegenerative diseases, such as Alzheimer’s (AD) and Parkinson’s (PD) diseases. Instead of the accumulation of β-amyloid and tau for AD, it is alpha-synuclein in PD.
Synthesis
In the last decade a whole body of knowledge has emerged about the brain’s drainage system—glymphatics— and the accompanying key components of the system that efficiently rids us of unwanted molecular waste every day. The dramatic impact of non-REM sleep, particularly stage 3 slow-wave deep sleep, cannot be emphasized enough. Ironically, Ambien, a commonly used drug to help people sleep, backfires and actually suppresses waste disposal. There are likely many other drugs that are either used for sleep aids or are associated with sleep disruption that have similar adverse effects. Ambien, a benzodiazepine like Valium, and other sleep medications have been associated with a heightened risk of Alzheimer’s disease and dementia in multiple studies. While this link is not definitive or established as causal, the mechanism may well be the impairment of brainwashing (the vasomotor oscillations and norepinephrine pump function) induced by the medications.
With the new elucidation of this pivotal drainage mechanism, it is notable that none of the commonly used sleep medications or supplements have been shown to improve waste clearance, the principal function of sleep. Or promote deep slow- wave sleep without important side effects. We are in desperate need for effective and safe sleep medications that will achieve these objectives. One potential non-pharmaceutical technology is non-invasive brain stimulation to promote normal and synchronous neuronal oscillations.
For now, however, we have to rely on better behavioral and lifestyle factors to promote healthy sleep, the list you are familiar with, including maintaining regularity of bedtime and awakening, exercise, avoidance of late eating close to bedtime, avoidance of alcohol, especially within 3 hours of going to bed, a cool and fully dark bedroom, avoidance of blue light, diagnosing and treating sleep apnea if present, and relaxation training techniques or digital cognitive behavioral therapy.
The extensive glymphatic work reviewed here was predominantly accumulated in rodent models since such experiments would not be possible to obtain in people. However, we now have brain organ clocks, as previously reviewed, as a means to determine interventions that slow the pace of brain aging. Finding new ways to promote brainwashing as we age should be considered a high priority to help reduce the toll of neurodegenerative diseases in the future.
********************
Thanks for reading and subscribing to Ground Truths.
If you found this interesting please share it!
That makes the work involved in putting these together especially worthwhile.
All content on Ground Truths—its newsletters, analyses, and podcasts, are free, open-access.
Paid subscriptions are voluntary and all proceeds from them go to support Scripps Research. They do allow for posting comments and questions, which I do my best to respond to. Many thanks to those who have contributed—they have greatly helped fund our summer internship programs for the past two years.






Fascinating, isn't it!? I wrote a post about this over the summer, and there is some evidence that perhaps the Glymphatic System works most efficiently when we are sleeping on our sides.
https://mccormickmd.substack.com/p/is-there-a-better-head-position-for
The reporting that even one night's poor sleep can result in amyloid deposition is sure to stoke fear and catastrophic thinking among those who are troubled by their insomnia, and obsess over the damage they are being told this causes. It's great your article highlighted that the relative risk of dementia is still cumulative, and even with less than 6 hours sleep on average over 25 years, the risk is "only" increased by 20%.
The body knows best. Another study found that naturally we are inclined to sleep more on our sides, likely to facilitate best positioning for the glymphatic system to work, in addition to orthopedic issues, spinal alignment, etc.
The link I posted above also contains a YouTube video showing the blood flow, CSF dishwasher cycle in full effect!
Cheers. I'm glad the Glymphatic System is indeed newly discovered, as I worried that perhaps in medical school I had slept through that lecture ;)
Glymphatics.. the brain mechanism for "flushing"... Fascinating stuff. I wonder if there is something about Long COVID short term memory loss that could be due to something "broken" in this process?