When we published our comprehensive review of Long Covid earlier this year, the evidence for elevated risk of autoimmune diseases had not been established. That’s now changed. There are three large cohort studies that provide strong support of the “substantially increased risk of developing a diverse spectrum of new-onset autoimmune diseases.”
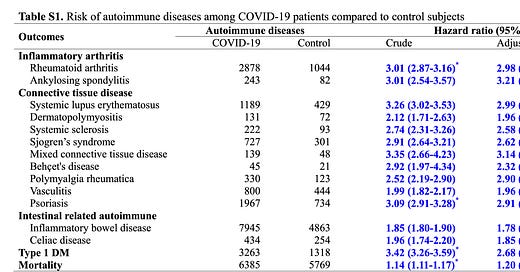
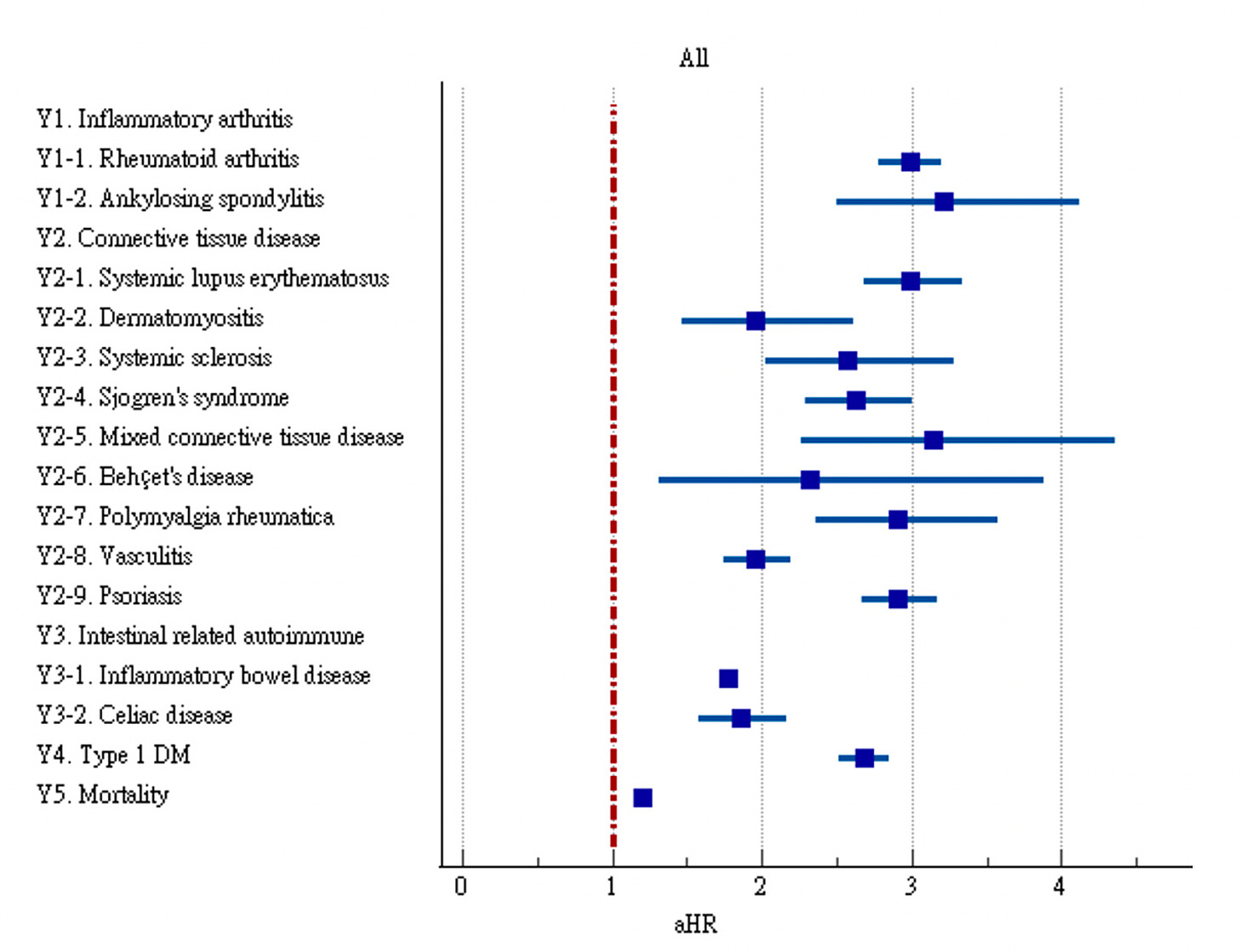
The Table below is the summary of the 3 reports (here, here and here) that come from 3 different countries, each with matched control groups. The increased risk of multiple new autoimmune conditions is fairly consistent, about 20-40%.
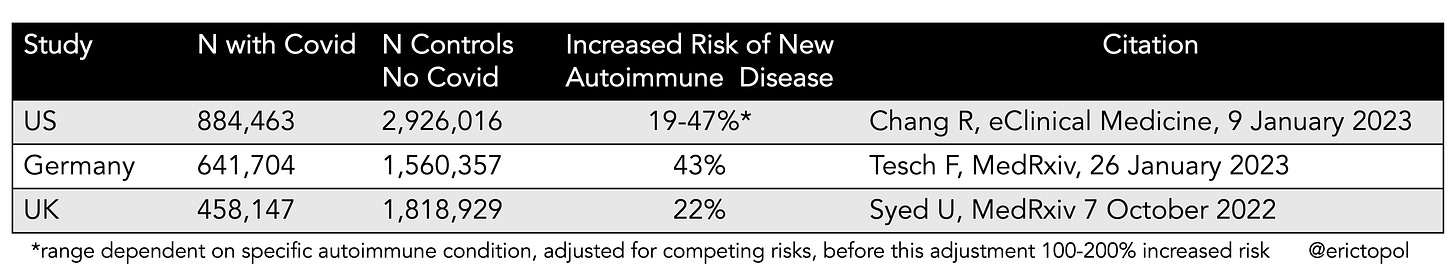
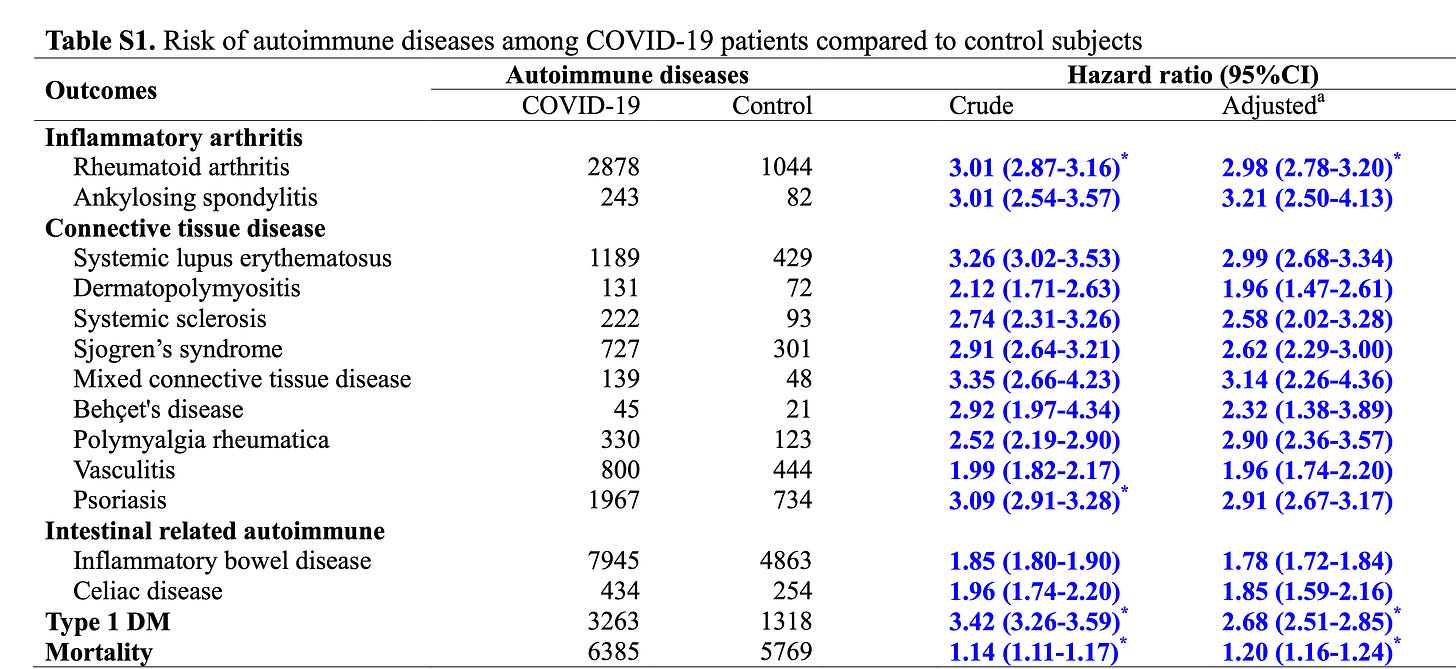
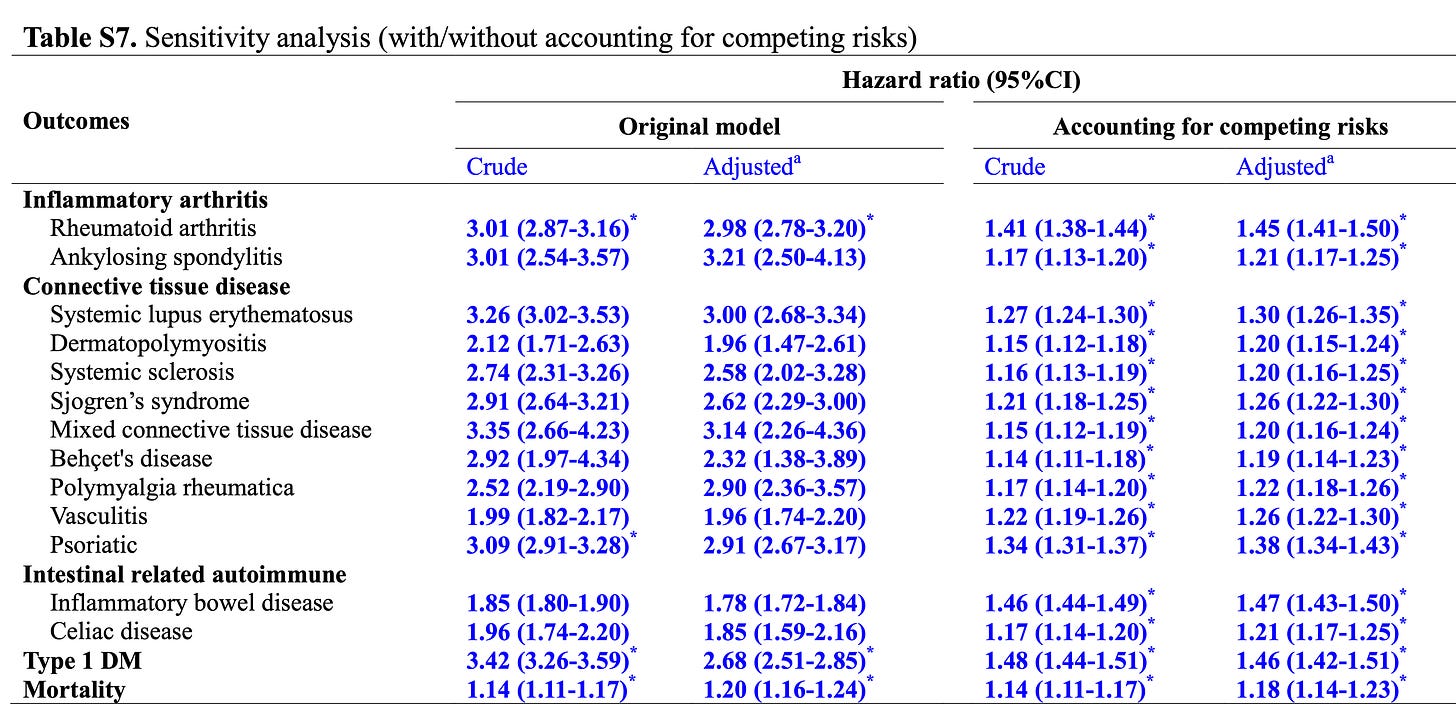
The analysis of the data from the United States is notable because it considered and adjusted for competing risks, that is one or more severe outcomes that could compete with the outcome of interest. Before this adjustment, as seen below, the risk for the spectrum of autoimmune disease ranged from about 2-3 fold (hazard ratio at far right, adjusted).
And here is the corresponding Figure
When competing risks were factored in there was still a significant increased risk, but more in keeping with the other 2 reports (20-40%). The cohort analyzed excluded any individual who had received a Covid vaccine.
The analysis partitioned the cases and controls as to whether they had severe Covid (hospitalized) or were out-patients. The risk was more elevated in the people with mild to moderate Covid, as seen below. Somewhat surprising, given the higher incidence of autoimmune disease among women and younger age groups, there were no substantial overall differences noted by age, sex, or race, but specific autoimmune diseases did vary (e.g. Behcet’s disease, dermatomyositis, systemic sclerosis and mixed connective tissue disease excess only found in women; systemic lupus erythematosus (SLE) in Asians; psoriasis and ankylosing spondylitis in Blacks). In contrast, the other 2 studies reported a somewhat higher incidence of new autoimmune diseases among women and the German study showed a higher risk among in-patients. None of the 3 reports had data for the effect of vaccination.
In contrast with respect to risk according to severity of Covid, the German study
The US report concluded: “Given the large sample size and relatively modest effects these findings should be replicated in an independent dataset.” Well now this finding has been seen in triplicate and it appears to provide unequivocal support for the link (an association, not yet established as cause and effect) between Covid and subsequent risk of developing autoimmune diseases.
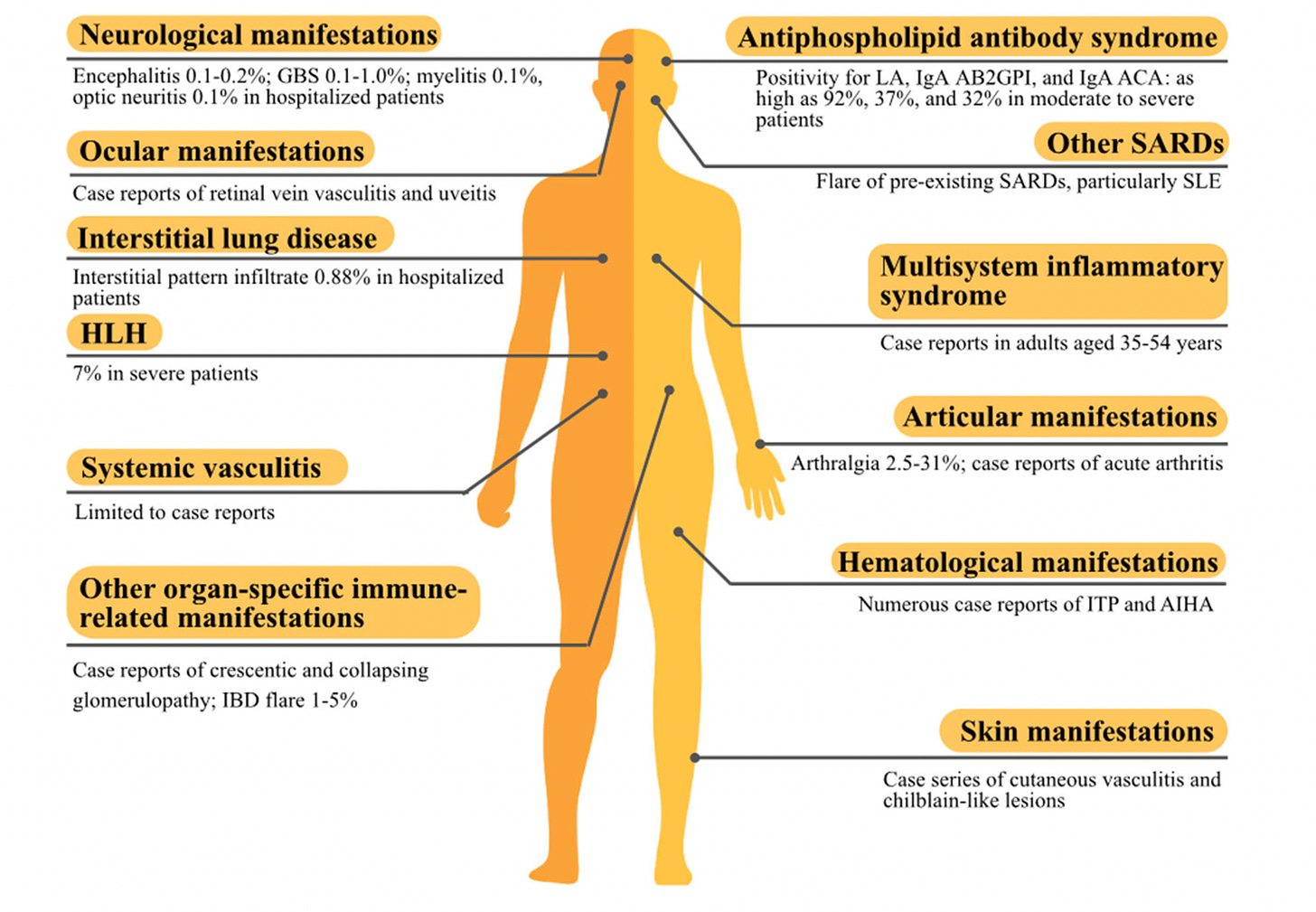
Birds of a Feather
We have been warned of this potential since the first year of the pandemic when there were multiple fronts of anecdotal data, case reports, and small series, as summarized in the Figure below. The findings included the rare Multisystem Inflammatory Syndrome in Children (MIS-C) and even less frequently seen in adults, the high proportion of antiphospholipid antibodies found in multiple studies, chiblain-like lesions (“Covid toes”), and hematologic conditions such as immune thrombocytopenia or hemolytic anemia that have an autoimmune basis.
The Autoantibody Story
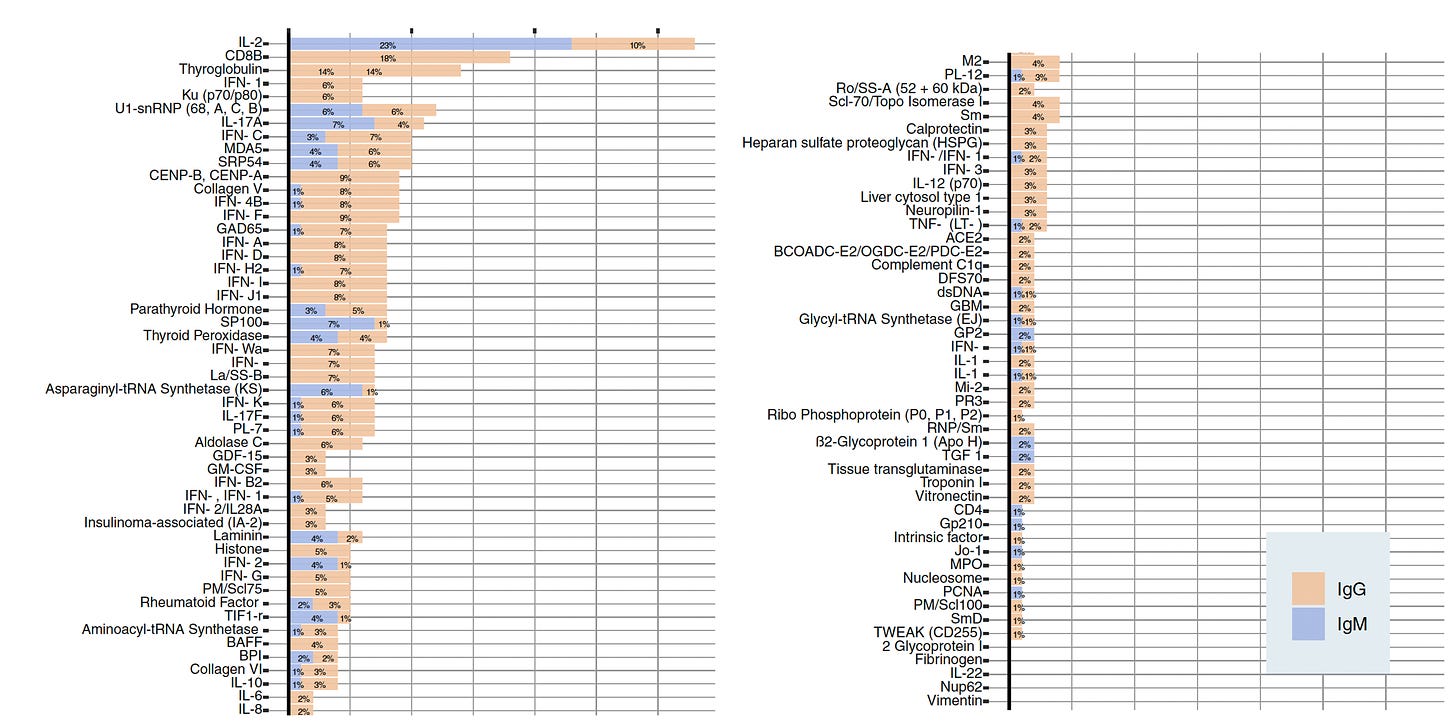
There are (so) many publications that highlight the multitude and spectrum of self-directed antibodies (autoantibodies) after Covid, such as this one, both IgG and IgM, with proportion for each.
Of note are the extracellular, non-SARS-CoV-2 autoantibodies, especially directed towards herpes viruses, including Epstein-Barr (EBV), as seen below, in the report by Klein et al. While some of these autoantibodies can be present before Covid, this study provided evidence for their cropping up following Covid and their functionality. Autoantibodies after viral infection are not unique to SARS-CoV-2 and have been seen after multiple viruses, and in patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). Reactivation of a virus, such as EBV, is thought to be one of the possible underlying mechanisms for Long Covid, ME/CFS, and autoimmune diseases.
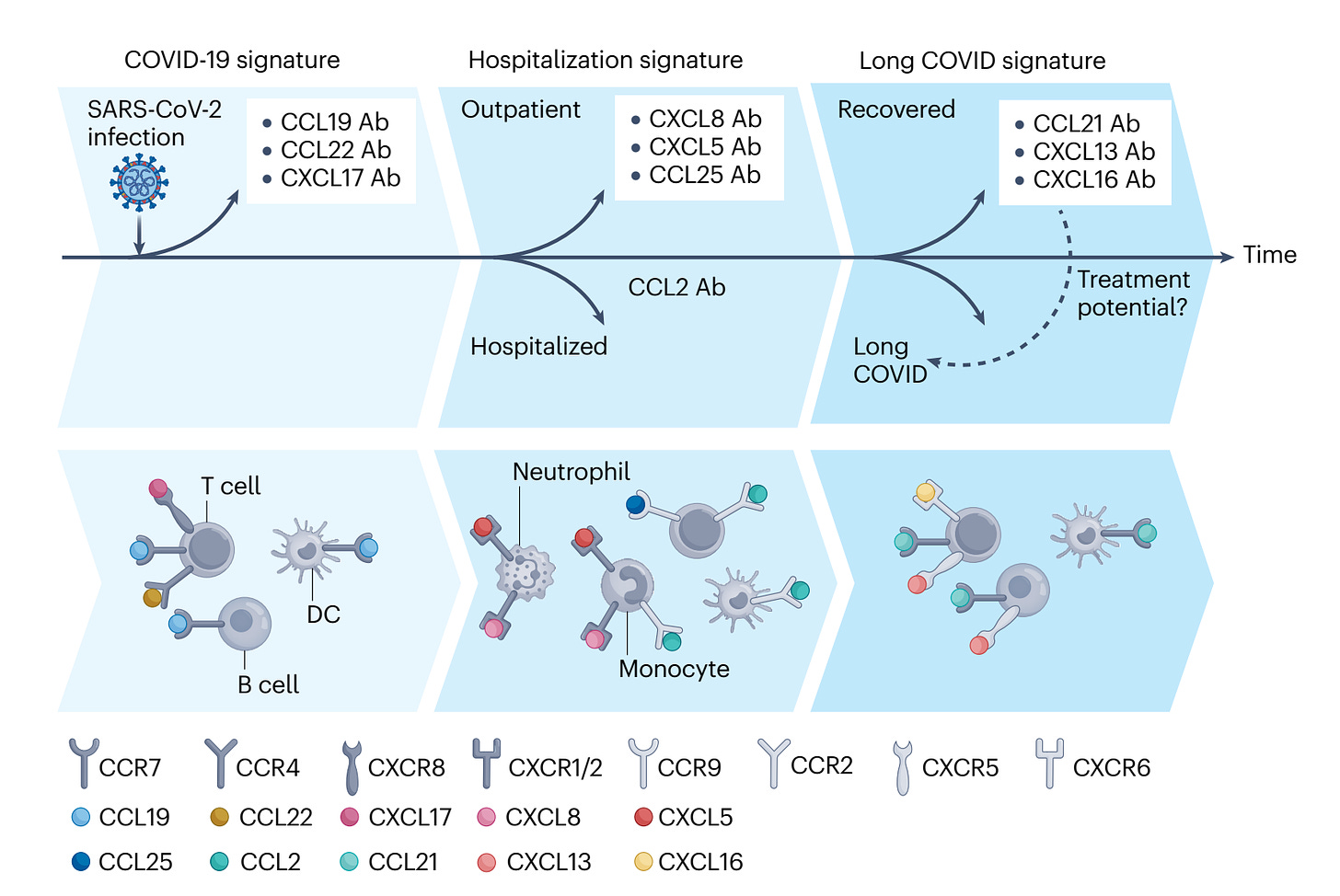
These autoantibodies are not all bad. One recent report showed the protective impact of autoantibodies directed against specific chemokines (proteins secreted from cells) (Figure below)
Some of the autoimmune conditions that have arisen after Covid have also been seen after Covid vaccines, while quite rare, they include rheumatoid arthritis, Type 1 diabetes, SLE, and autoimmune polyarthritis.
Why are these findings important?
Previously we knew there were many features of autoimmunity engendered by Covid, but the link to manifesting important autoimmune diseases has not been established. There are still many dots not connected—it’s fuzzy. We need to better understand how the dysregulation of our immune system that can occur from a Covid infection (or even more rarely from a vaccine) can be linked with a serious autoimmune condition. While we’ve fully recognized that people with autoimmune diseases are more vulnerable to Covid and adverse outcomes, the flip of that—that Covid can make some people vulnerable to autoimmune diseases—is what’s new.
Thanks for reading, sharing and subscribing to Ground Truths!
The proceeds from all paid subscriptions will be donated to Scripps Research.