The SARS-CoV-2 variants successively keep finding new and repeat hosts, now more efficiently than they did before, despite so many prior infections, vaccinations, and boosters. Reinfections with BA.5, while poorly tracked, are likely occurring at the highest frequency in the pandemic, whereas through the Delta variant wave the chance was less than 1 in a hundred of getting Covid a 2nd time. The infectiousness period of BA.5 appears to be longer by a matter of days, although not adequately or fully quantified, giving hosts a better chance of spreading their infection.
Yet the perception is that there is a low rate of fatality, ICU admissions, and hospitalizations relative to Omicron BA.1 and previous variant waves. That is not because the pandemic is fading away. It is attributed to building our immunity wall from millions of infections, vaccination doses and boosters. The wide use of Paxlovid may even be adding to keeping the rate of US hospitalizations lower, with the perception they are not alarmingly high, at over 40,0000 (and far less than 160,000 at peak Omicron BA.1) but still rising. Don’t forget the enormous toll of Long Covid that isn’t going away as the virus has evolved to Omicron and it subvariants, as reported today.
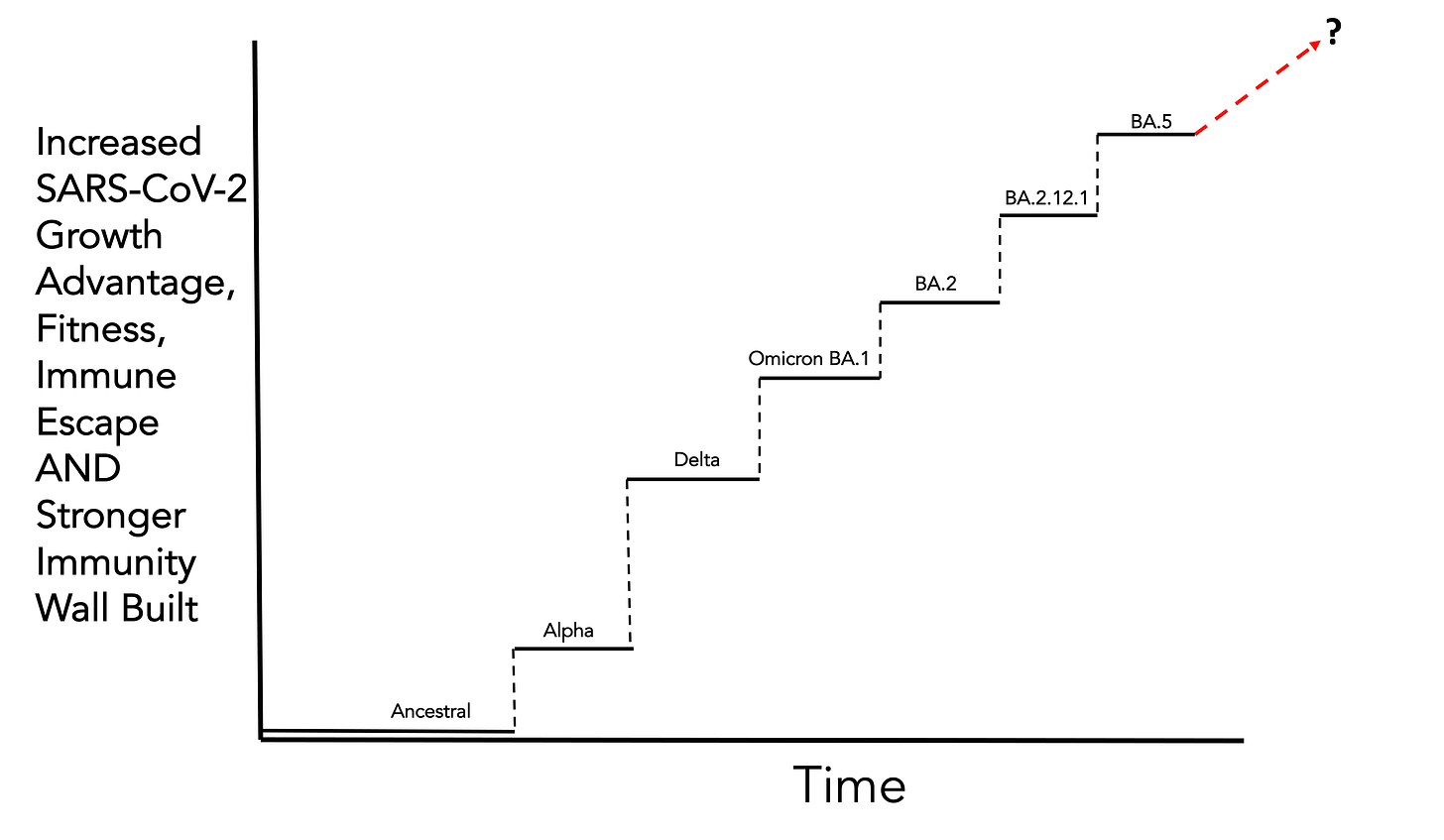
Thus, we have 2 major, concurrent, opposing trends that are obfuscating the real arc of the virus’s evolution and impact. On the one hand, the virus is getting more fit (defined as the composite of lineage growth, basic reproduction number, extent of immune-evasion and generation time), greater growth advantage, and immune escape properties that have culminated in the BA.5 variant which I maintain is the worst form of the virus—not because it has raised deaths or hospitalizations to a high level, but owing to its unprecedented level of immune evasion (by multiple mechanisms that include suppression of innate immunity) along with its heightened infectivity of cells. The mutations it has acquired beyond Omicron BA.1, BA.2, BA.2.12.1 make it even more formidable, and help explain why it is achieving global dominance. We’re down to one effective monoclonal antibody that still is effective vs. BA.5 for treatment and even Evusheld, the combination monoclonal antibody for protection in the immunocompromised population has lost some efficacy with BA.5.
It looks like this.
It’s a gradual process whereby over time one new variant out-competes another because of its biological and host-seeking/infecting advantages, while at the same time human infectees, vaccinees, and boosterees are better fit to withstand the ill-effects of the virus. That makes people think it’s more “mild” and less of a threat, when it fact the pressure that is being put on the virus is making it more formidable as time goes on. But now BA.5 has progressed to such a point that even people with recent BA.1 or BA.2 infections are getting hit again, and our vaccines, even with 3rd and 4th shots, are unable to meaningfully block infections or spread. And there’s inevitably more evolution to come, with tens of millions of immunocompromised hosts around the world, spillovers to humans from multiple animal reservoirs, and uncontained spread of the virus throughout the world with many new recombinant/fusion variants documented by sequencing.
The Gradual Attrition of Protection
The new CDC report from 15 July is worrisome. Look at the attrition of protection vs hospitalization between BA.1 and BA.2/BA.2.12.1 for more than 58,000 US hospitalizations during the Omicron wave ranging form December 2021 to mid-June 2022.
To quote the CDC press release:
“When BA.1 was the predominant variant, vaccine effectiveness (VE) was 61% for two doses against COVID-19-associated hospitalizations; VE increased to between 85%-92% after a receipt of a third/booster dose.
When BA.2.12.1 became predominant, vaccine effectiveness with two doses was 24% against COVID-19 -associated hospitalizations and increased to 52%-69% after a third/booster dose.”
The title of the press release was “New COVID-19 Vaccine Effectiveness Data Showcase Protection Gained by 3rd and 4th Doses”
While that’s true, it was well established by multiple prior reports as I have previously summarized, the more striking concern is a near 40-point drop for protection vs. hospitalization for people with the primary vaccination series (2 doses) and inability to restore to the same level of 92% with a 3rd dose as for BA.1.
Could this be because the reference group of unvaccinated have had a lot of infections making the gradient of protection less? Yes, but there’s no shortage of breakthrough infections among the vaccinated in this period of time with hybrid immunity adding strength of protection. There was increasing use of Paxlovid which is a confounder that reduced the need for hospitalizations. Importantly , these are large reductions without any changes in categorization for what is “for” or “with” Covid hospitalizations during this same time period. Even accounting for these uncertainties, the gap is far bigger than has been previously noted since vaccine effectiveness studies have been reported. Further, it is replicated by a decline, albeit to a lesser degree, from Delta to BA.1 to BA.2 in vaccine effectiveness in the Kaiser Southern California datasets . It wasn't seen in the UKHSA comparison of BA.1 and BA.2 posted March 24, but recall there was no appreciable BA.2.12.1 seen there or in the Kaiser report. Indeed, I suspect the attrition noted in the new CDC report is indexed mostly to BA.2.12.1 which had the L452Q mutation and, largely as a result of this change, had more immune escape than BA.2 (or BA.1).
We have no vaccine effectiveness data yet for BA.5.
If we turn to the boiling frog apologue “The premise is that if a frog is put suddenly into boiling water, it will jump out, but if the frog is put in tepid water which is then brought to a boil slowly, it will not perceive the danger and will be cooked to death.” No, we’re not going to get cooked and deaths won’t rise anywhere near the 4,000+ per day levels we have previously seen. But we’re not adequately perceiving the threats that the evolving virus is presenting to us: its fitness is gradually getting enhanced and this is happening at the same time as a constant building of our immunity wall. In fact, they are tightly intertwined. Just imagine if we were hit with BA.5 before BA.1.
Why do I remain optimistic? Because SARS-CoV-2 is a much easier virus to prevail over than influenza. We have never had a flu vaccine with 95% efficacy; we’re lucky to have multivalent ones that are 40% effective. Tamiflu is a weak hitter compared with Paxlovid. The virus’s main protease (Mpro) makes for an enviable choke point to take it down SARS-CoV-2, even though resistance to the drug from mutations in Mpro will likely manifest in the months ahead. Although the mutations with functional consequences have been considerable with SARS-CoV-2, they are minimal compared with the head of the influenza virus. Variant-proof “universal” coronavirus vaccines and nasal vaccines to block transmission and infection are our way to turn off the heat and get ahead of the virus’s evolutionary arc. We know what we need to do; we’re just not doing it. The boiling frog metaphor is contributing to the lack of taking action.