There has been a flood of new data in the past few weeks regarding Omicron’s impact throughout the world, and specifically on the influence of vaccination (with or without boosters) on symptomatic infections, hospitalizations, and deaths, including durability. It’s actually remarkable how much and how quickly we are learning about Omicron and our ability to reduce its toll, considering this virus strain was reported less than 2 months ago.
The New Data
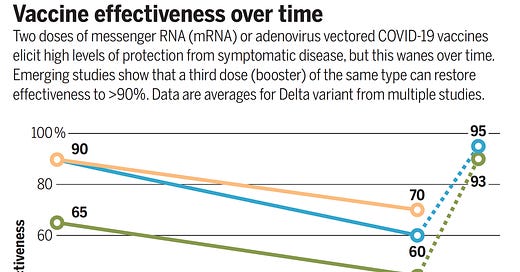
Clearly, there’s a major problem with vaccine breakthrough Omicron infections. Recall that with a booster vs Delta, the vaccine effectiveness was restored to ~95% as Ravin Gupta and I recently reviewed all of the reported studies in Science
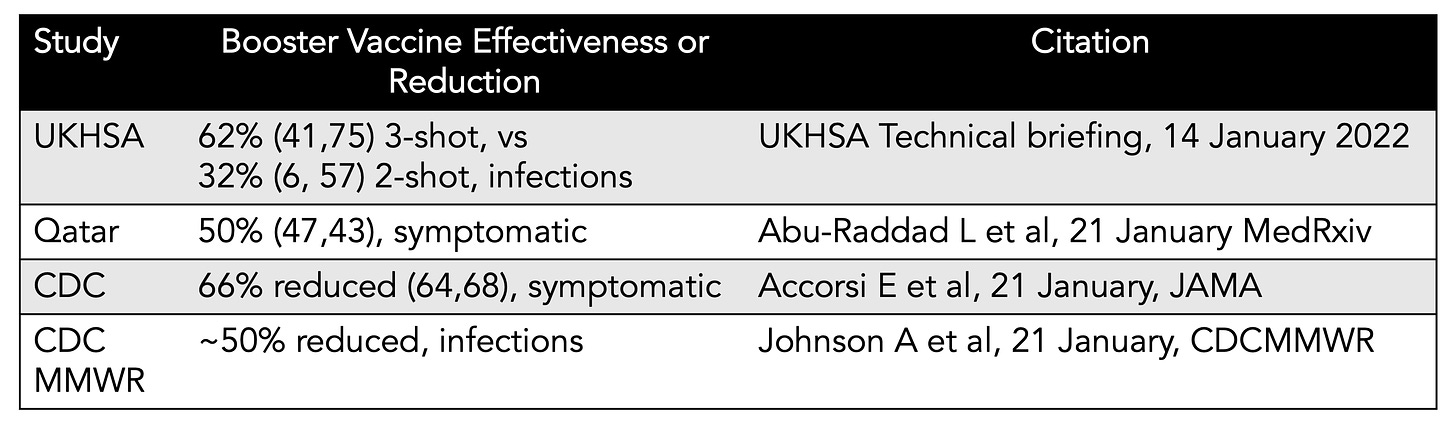
The problem with the booster with Omicron is that instead of getting vaccine effectiveness vs infections (symptomatic or all) up to 95%, it is about 50% from 4 new reports, summarized in this Table. To date, the best study comes from Qatar with over 400,000 people boosted with either Pfizer or mRNA
Here are the Qatar study data with clear diverging curves, albeit with limited time of follow-up. We’ll get to the issue of durability below, where there’s available data.
The Math
That level—about 50% effectiveness for the booster (vs Omicron)—would be associated with 10-fold more breakthrough infections than seen with a 95% effectiveness (Delta) So it’s no wonder there is the public perception that Omicron breakthroughs are omnipresent, that “vaccines aren’t working”. They aren’t working well, but it isn’t true that they’re not working to protect vs infections and transmission. It’s just much less. For context, remember that the FDA criteria for approving a Covid vaccine was set at a 50% reduction of symptomatic infections, so there’s unquestionably some efficacy here, just not nearly what we’ve been accustomed to seeing.
As I was quoted in the Washington Post coverage, “A booster is essential for preventing severe disease, hospitalization and deaths,” said Eric Topol, a molecular medicine professor at Scripps Research, referring to the findings. Public health officials need to communicate clearly that although the vaccines and booster shots are “not holding up against omicron infections, they are holding up the wall against severe disease … and that’s phenomenal.”
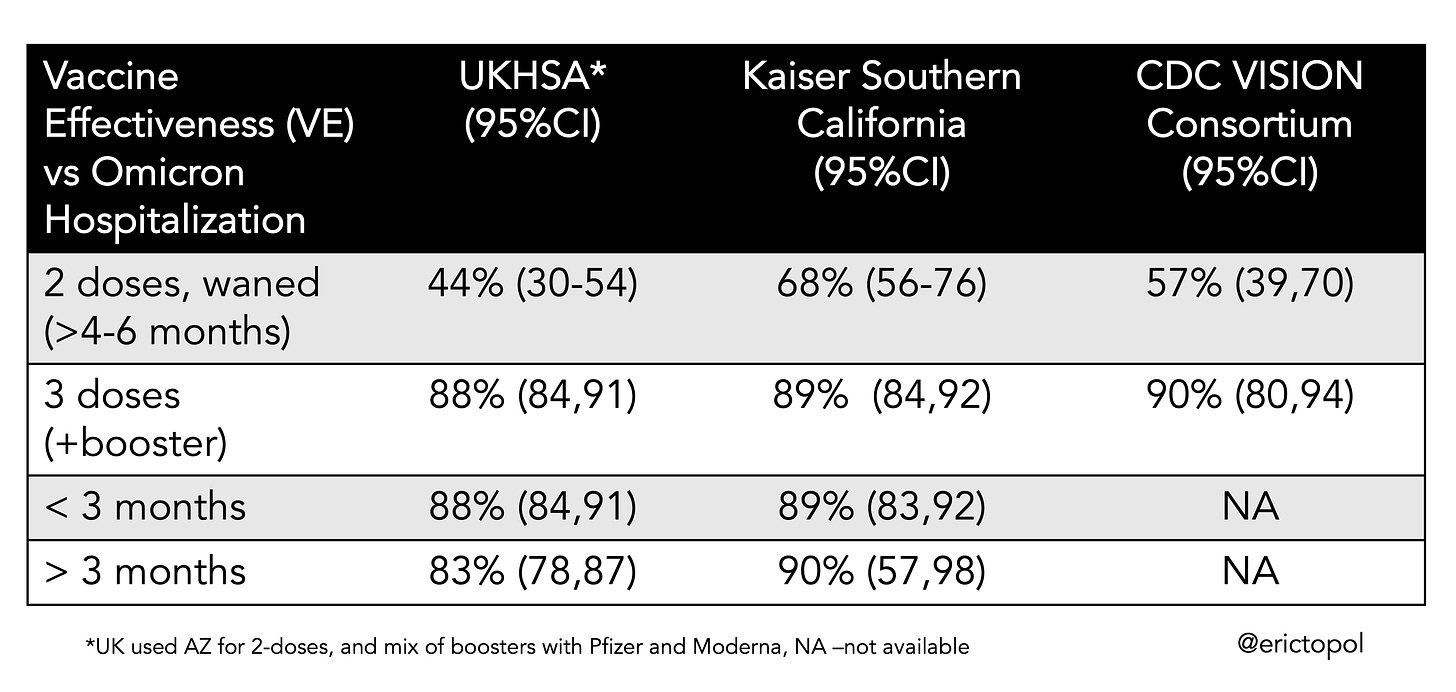
Now let’s turn to hospitalizations where the data are extraordinary, consistent, potent protection, and by all we have to go on, very durable. There are 3 reports: the UKHSA, the Kaiser Permanente Southern California, and the new CDC MMWR as summarized in this Table. It is exceptionally rare to see such consistency in triplicate—88, 89, and 90 for booster effectiveness vs Omicron. That is substantially improved compared with 2 shots (44-68%). And, importantly, it appears to be quite durable (83-90%) after 3 months, an attrition level fully in keeping with what we have seen over time with the Delta variant. As I previously wrote, We’re very lucky. Damn lucky.
This new CDC graph compares the effectiveness of vaccination with or without a booster against Delta and Omicron hospitalizations. The 3rd dose gets to near parity for the 2 strains even though Omicron is the most immune evasive variant we’ve seen., with far more extensive waning of protection that with Delta.
There really is an Omicron booster vaccination dichotomy—protection vs infections vs protection vs severe disease (hospitalizations and deaths)—that has led to much confusion. The booster’s effect is dual: it induces neutralizing antibodies at high levels and expands memory B and T cells as previously reviewed. The latter is what really accounts for protection vs severe disease, and that also would be expected to be quite durable. Which makes the case that the 3rd shot may be long-lasting for such benefit, at least against Omicron. Early in the pandemic we focused on symptomatic infections (there primary endpoint of the pivotal clinical trials) since they tracked so closely with severe disease outcomes. That relationship markedly changed with Omicron; they are now dissociated to a substantial degree.
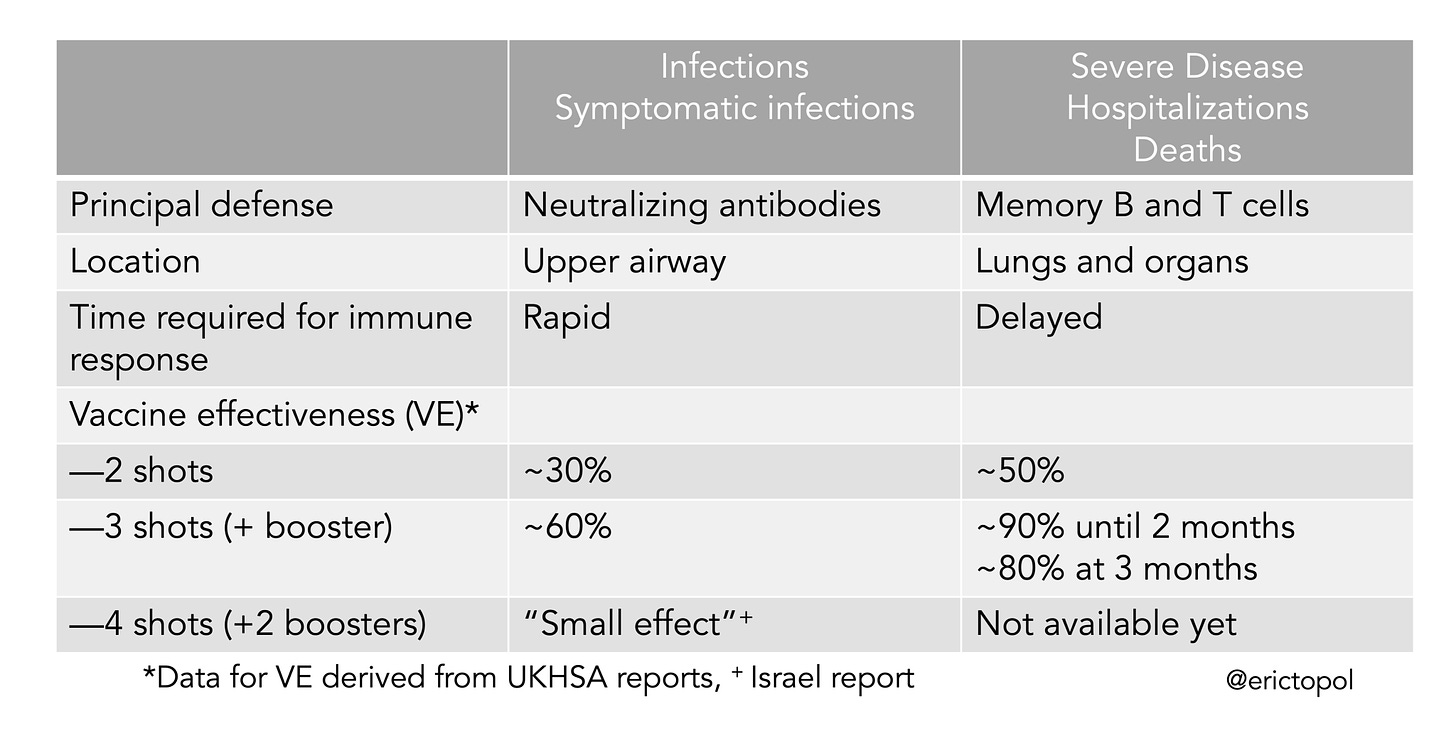
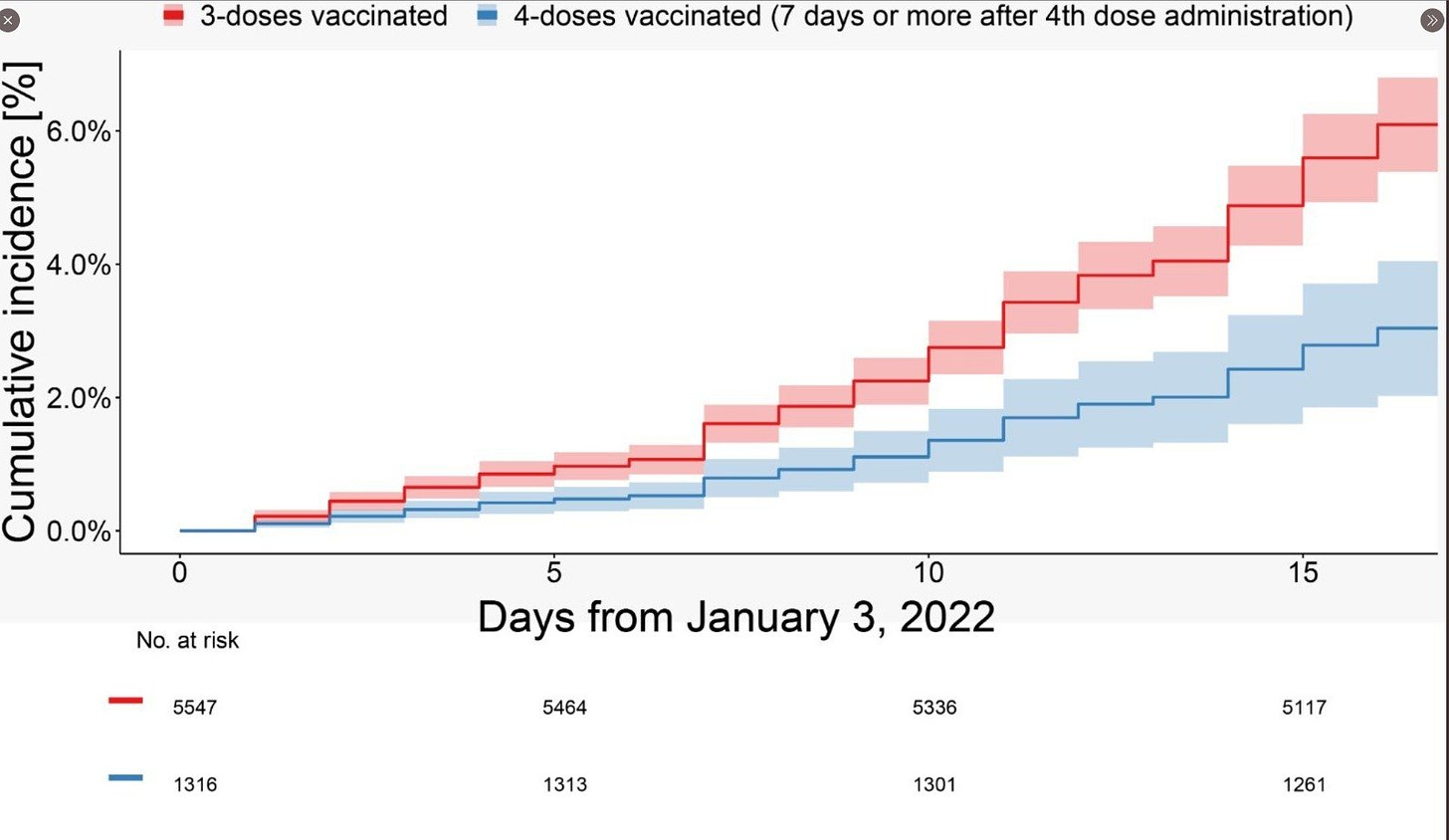
The new Israeli data for a 4th dose (2nd booster) vs the initial booster during its Omicron wave shows a similar pattern of reduction of infections (very) short term, but we await data regarding hospitalizations and deaths, which are incubating.
The Patterns
It is quite clear in reviewing the patterns from some of countries hit hard by Omicron that vaccination and booster rates are playing a critical role in keeping severe disease in check. One example is Portugal, with 90% 2-shot vaccinated and over 40% boosted. New cases have gotten extremely high during its Omicron wave, but the impact for ICU admits or deaths, fortunately, has been small to date.
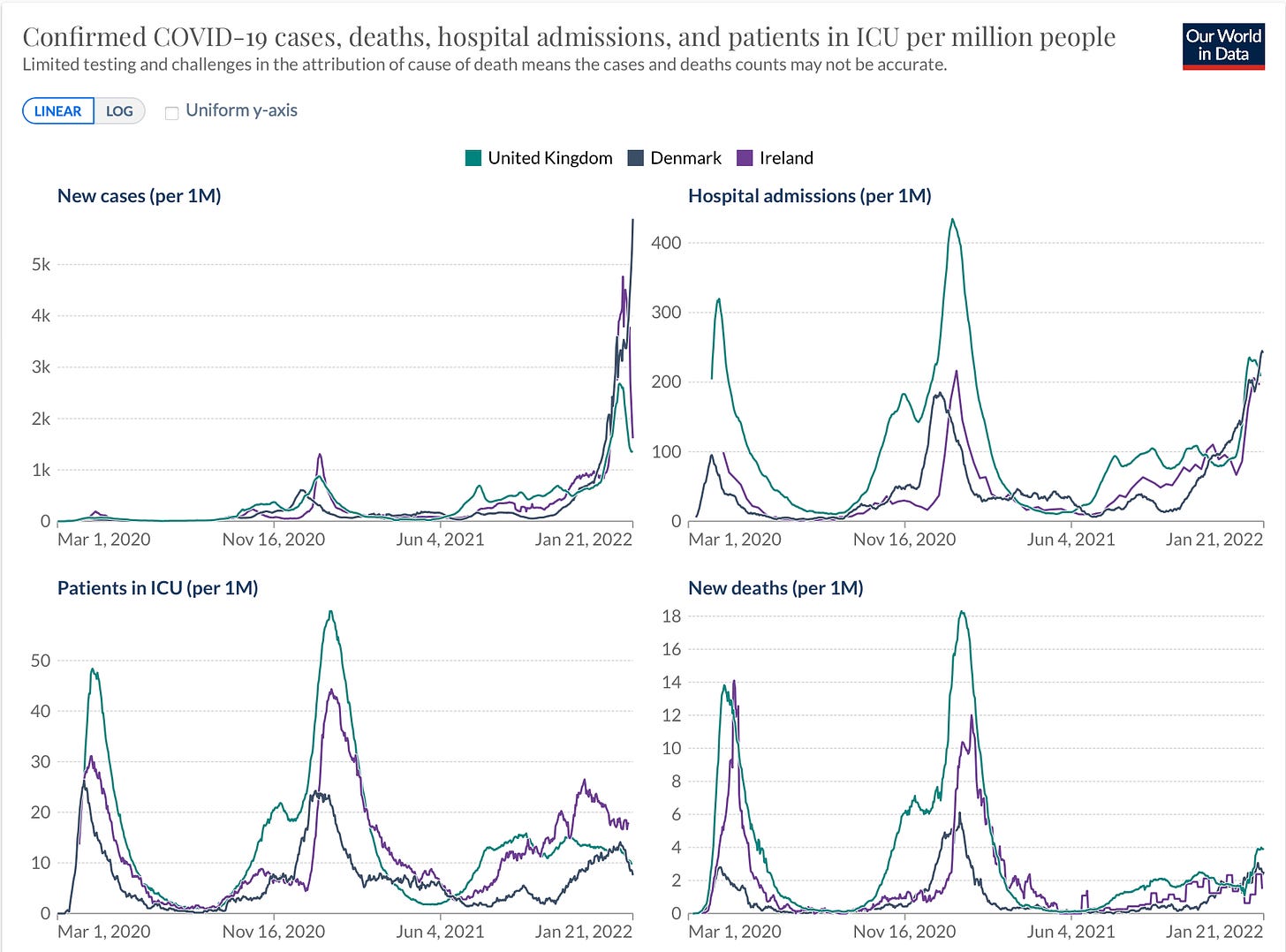
Similar patterns, perhaps less pronounced with respect to the case vs ICU/deaths dissociation, are evident in Denmark, Ireland, and the United Kingdom, all going through Omicron waves.
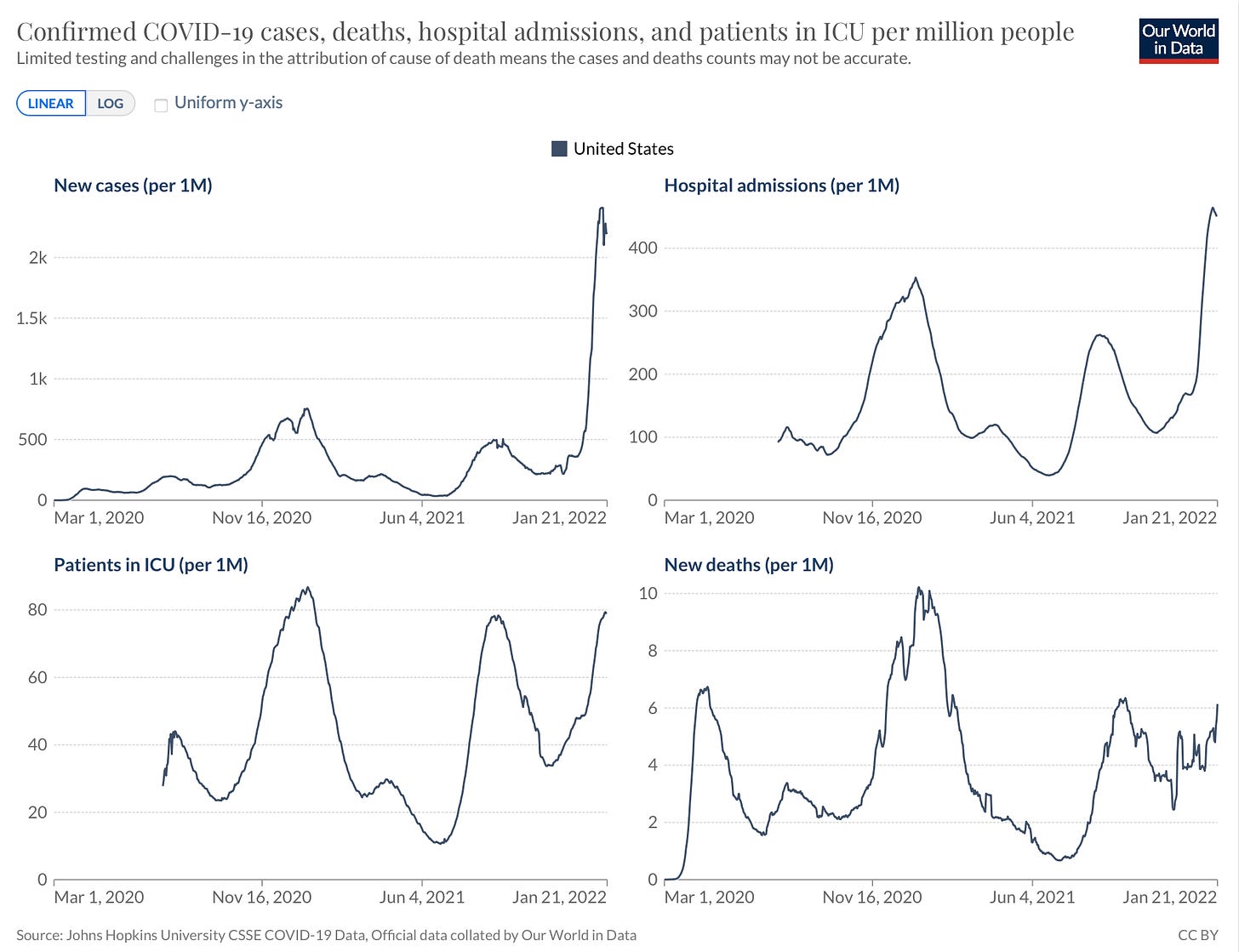
However, this is a very different look from the United States, where hospitalizations have soared to a new record, ICU admits are close to their pre-vaccination phase peak, and deaths are again on a steep rise (nearly 4,000 reported yesterday, one of the highest for the US pandemic). These severe disease outcomes are likely a function of very low vaccination rates (63%) and booster rate (24%) compared with the European countries cited. It is also noteworthy that the United States was into its second Delta surge at the time when Omicron emerged in December, so these increases are superimposed. Further, in comparison to South Africa and some other countries, there are different demographics, such as age, and co-existing conditions, such as obesity or diabetes.
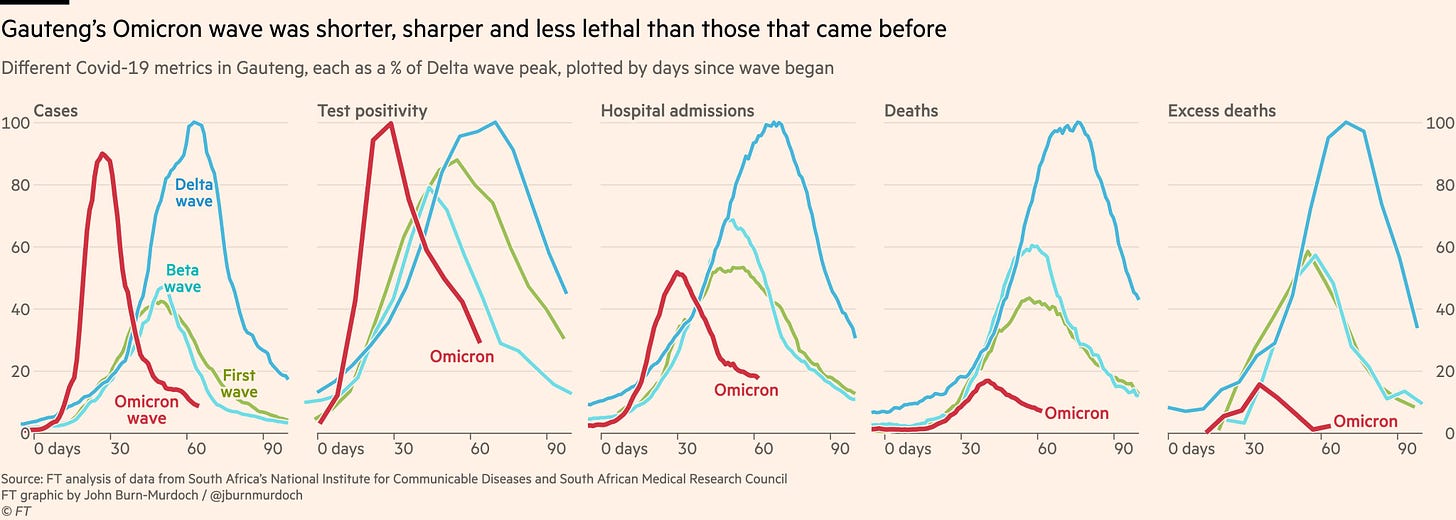
There’s been a lot written about Omicron’s sharp case descent, which was seen in Gauteng and throughout South Africa. But it isn’t so clearcut in other countries yet, especially normalized for reduced testing. It actually is somewhat wobbly, stuttering in the United Kingdom, one of the first countries outside of South Africa to begin its descent. So Omicron’s future trajectory isn’t clear, and we cannot rule out 2nd surges of Omicron at this point in places around the world. That occurrence may be influenced, at least in part, by the immunity wall built prior to and during the Omicron wave (from prior Covid, vaccinations and boosters), and only time will tell.
The Exit?
So where do we go from here? Is Omicron, by infecting “up to half the world’s population” going to serve as our exit ramp from pandemic to a contained, endemic state?
That isn’t clear and it would be foolish to predict that, even though that occurred this week Omicron’s going to help in building an immunity wall, but whether that will be sufficient is indeterminate. We’re so far from containing the virus at this point, enabling further accelerate evolution to a new variant that could potentially have a higher level of immune evasion (not so lucky as with Omicron), more fully evading our current vaccines, or even the Omicron-specific vaccine expected later this year.
That is why it’s so essential to push on the pan-coronavirus vaccine, oral and nasal vaccines that build mucous immunity and help block transmission, and get mass production of Paxlovid along with other safe and effective anti-Covid pills that are very likely variant-proof, not relying on our immune system.
As the Washington Post editorial board wrote today, and which I’m in total agreement":
“Ultimately, in chasing variants, we are always going to be behind the curve. Along with the immediate battle with omicron, renewed effort must be made to develop next-generation vaccines that will provide broader and longer protection and dampen transmission. Ideally, scientists will develop a universal coronavirus vaccine that encompasses all of these characteristics, capable of protecting against many — or all — known variants. That day cannot come soon enough.”
Now is not the time to rely on sharp descents and that somehow “it’s over". If that happens, and we quickly get to containment and low levels of circulating virus that are no more threatening than annual flu, terrific. It seems quite unlikely with so much of the world’s population, especially in low and middle income countries, have yet to be vaccinated. If there's one thing we learned about predicting the path of SARS-CoV-2, it’s that it’s unpredictable. So we shouldn’t plan on a rosy picture. There’s too much we can do right now to seize control in case the most optimistic scenarios don’t play out.