For recent developments in the world of Covid, there’s a lot to summarize.
The JN.1 Variant
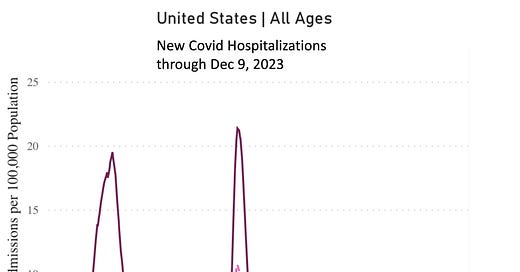
As predicted, it has become dominant globally. Its rise has been associated with marked surges in wastewater levels in many countries, as previously noted, and a substantial increase in hospitalizations in certain places (e.g. the Netherlands, Singapore, Île-de-France). We’ve not reached the 50% threshold in the United States yet, but that is expected in the next couple of weeks (←follow Jay Weiland @jpweiland for accurate forecasts), when we’ll learn the true clinical outcome (beyond cases and wastewater levels) of this variant here. Marc Johnson has raised the possibility that the very high increases in wastewater levels may be attributable to differences in tracking methodology, which would be a far better explanation than true virus burden. Let’s hope we’ll not see a major wave, which I suspect is the most likely scenario. We’ve already had an increase in Covid hospital admits, now above 23,000 per week, and that rise is mainly accounted for by people age 70 plus.
Good News on the Booster
A timely update from the Center for Infectious Disease Control in the Netherlands provided solid evidence for the monovalent XBB.1.5 booster (known by the CDC as “updated”) effectiveness. Prevention of hospital and ICU admissions for age groups 60 and above were quite high, as seen below. This is welcome news that correlates with multiple lab studies that provided unanticipated data for cross-reactivity of our immune response between XBB.1.5 and current circulating variants that include JN.1. If you haven’t had the booster (that would be most people, even in high-risk categories) you’d derive benefit for reducing the chance of developing severe Covid. Incidentally, a new report this week indicated that the survival benefit from primary vaccination waned after 6 months in older age groups, providing further support for the importance of booster protection.
Long Covid
The First Positive Randomized Trial
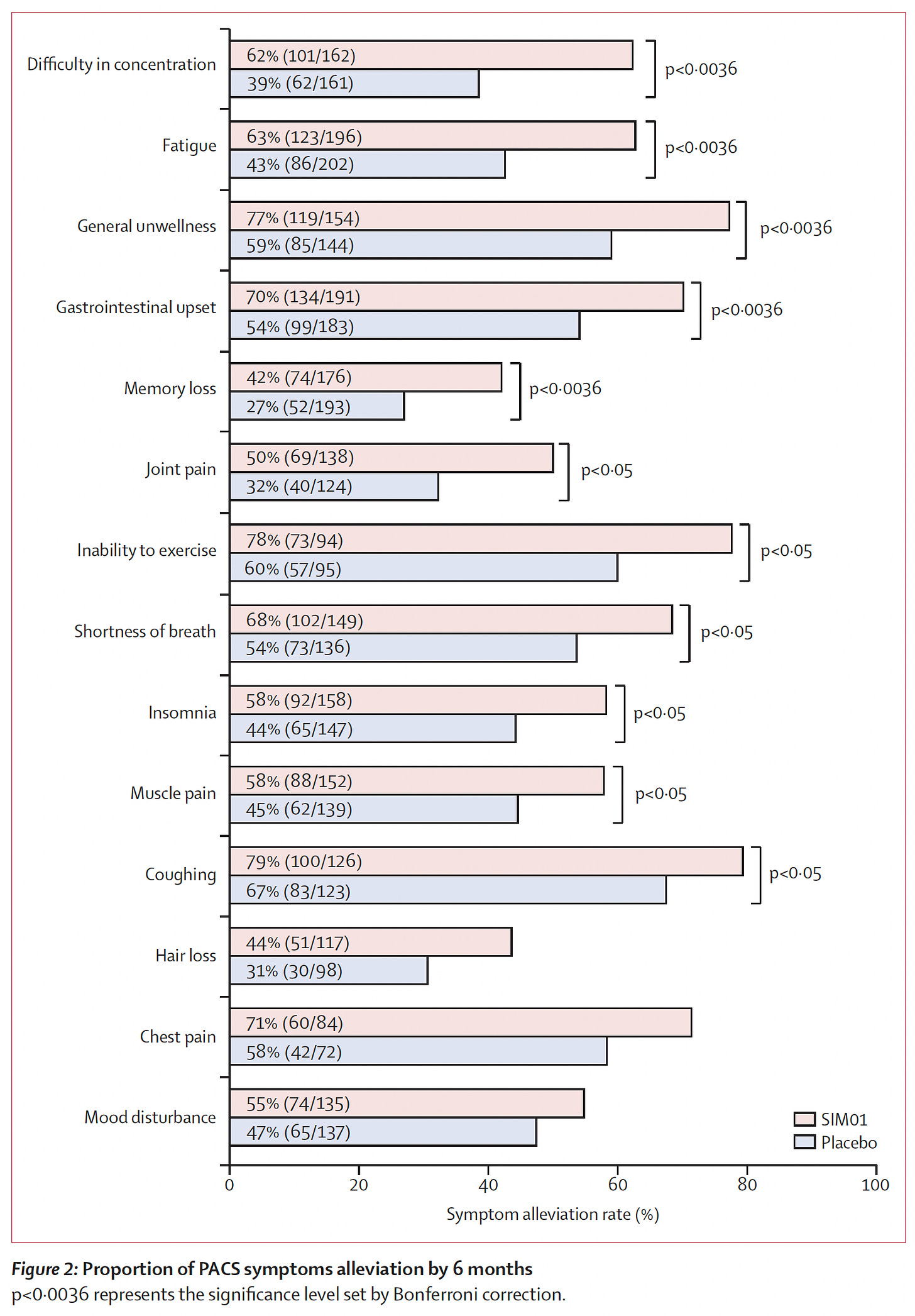
Last week researchers in Hong Kong published a randomized, double-blind, placebo-controlled trial of a gut microbiome intervention in 463 participants with Long Covid. This “synbiotic” preparation of combined pre- and probiotics, consisted of a “micro-encapsulated lyophilised powder containing 20 billion colony-forming units of three bacterial strains, B adolescentis, Bifidobacterium bifidum, and Bifidobacterium longum with three prebiotic compounds including galacto-oligosaccharides, xylo-oligosaccharides, and resistant dextrin.” It provided symptomatic relief at 6 months across most of the common and important symptoms of Long Covid, as shown below.
The mechanism of benefit is likely down-modulation of the immune response, for which the gut microbiome is a major driver, but that needs to be systematically assessed, along with larger trials in diverse populations to see if this microbiome modulation can be widely extrapolated. The benefit derived was incomplete, since the alleviation of symptoms (the primary endpoint) was not accompanied by improvement in overall quality of life as assessed subjectively. So even if this welcome positive trial paves the way for gut microbiome manipulation, it is unlikely to be enough on its own. No matter, such a positive result may be a hopeful turning point for Long Covid to become treatable in the future. Giorgia Lupi recounts her experience with Long Covid over 3 years in the New York Times this week. It’s an important read for people yet unfamiliar with the toll this illness takes and is representative of the undue, protracted suffering that so many people with Long Covid are going through.
Also this week: An outstanding Grand Rounds at UCSF on Long Covid with Akiko Iwasaki, Ziyad Al-Aly and Michael Peluso, moderated by Bob Wachter, can be seen here.
Long Covid vs Long Flu
The prolific Long Covid researcher —Ziyad Al-Aly—and colleagues published a paper comparing Long Covid and Long Flu in people who were hospitalized in the big Veterans Affairs data resource. There was a 50% increase in fatality among those post-Covid (compared with post-flu), as shown below, and the excess in organ-specific morbidity was across the board worse after Covid, along with impact on disability, with the only exception of pulmonary involvement for influenza.
Promising New Vaccines for Mucosal Immunity
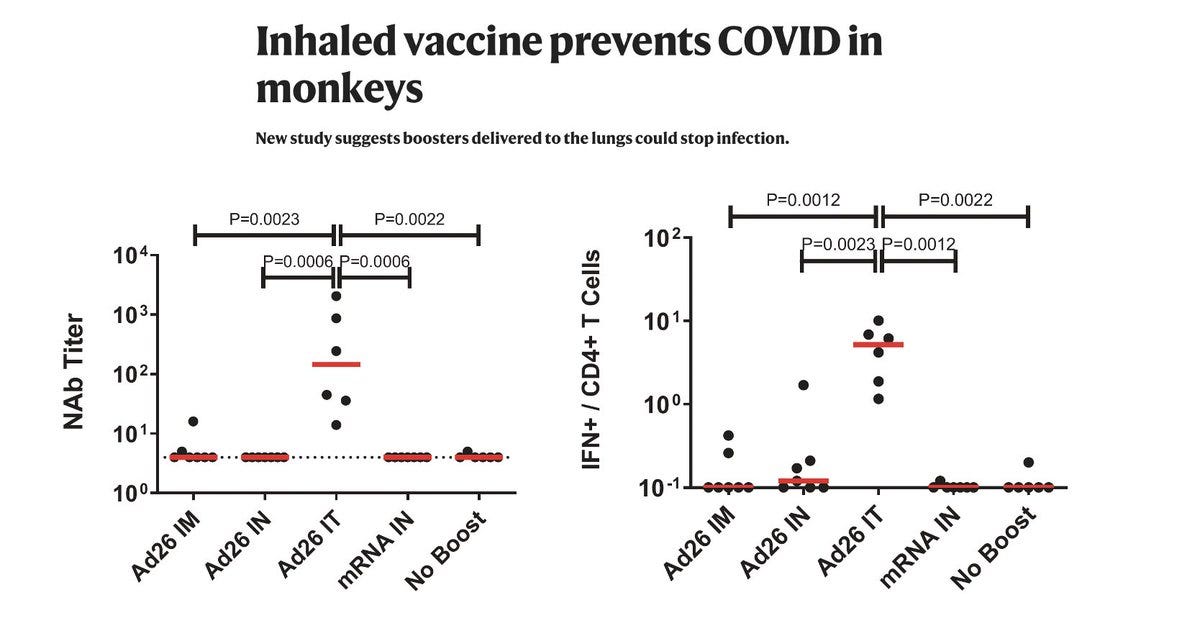
This has been an exceptionally positive week for new vaccines towards the critical goal of upper airway mucosal immunity, not achieved by shots, to help block infections and spread in the future.
An inhalation single-dose dry powder was effective in multiple species, including non-human primates, targeting the RBD antigen of the virus with a cholera toxin B adjuvant and nanoparticle package that does not have a cold-chain requirement. This protein-based vaccine elicited very high levels of RBD-specific IgA and IgG, local T cell response, and efficient protection against infection, including Omicron.
Another protein vaccine (bivalent Ad26, the adenovirus vector vaccine, univalent, used for the J&J shot) was given via the tracheal (IT) route (adaptable to inhalation) proved to be superior to shots (including Ad26 or mRNA) or intranasal for achieving humoral (neutralizing antibody) and cellular immunity, as shown below, along with providing near complete protection from infection after high-dose SARS-CoV-2 challenge (with BQ.1.1). If you like to get your information from podcasts, here’s one from Nature on the study.
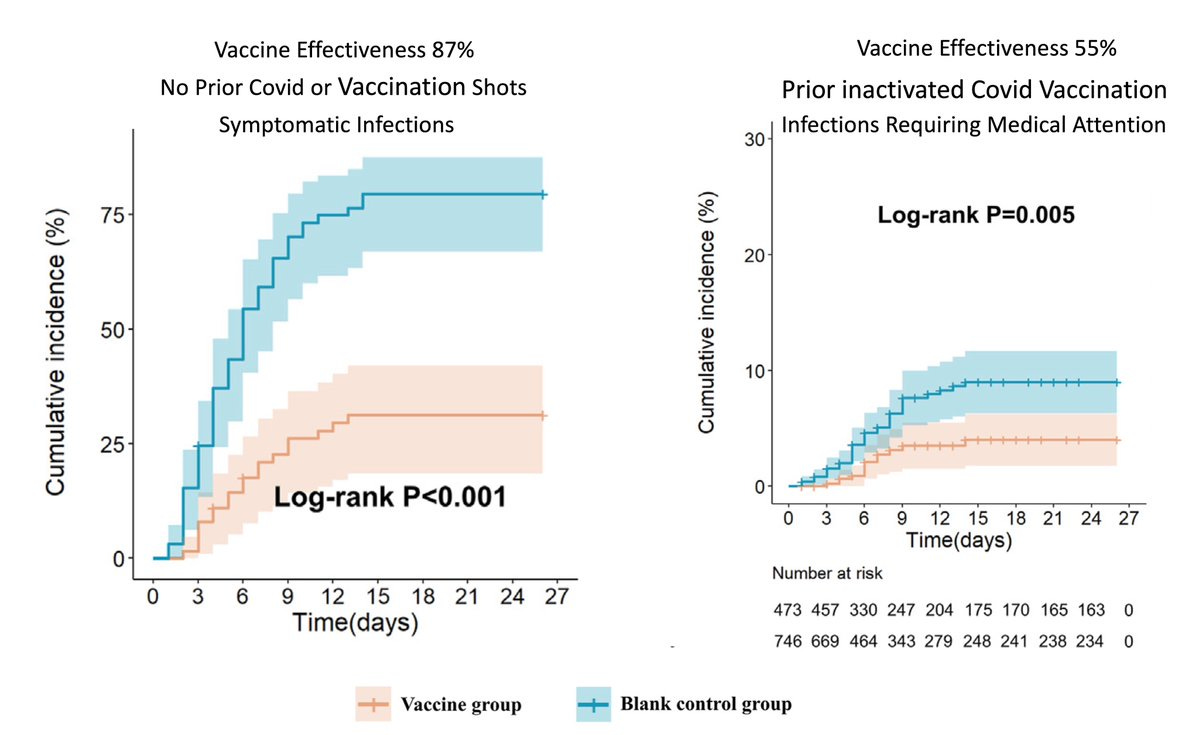
A prospective study among about 1,400 young healthcare workers (mean age 37 years) demonstrated short-term effectiveness of a single nasal spray vaccine during the Omicron wave in China. The inactivated Covid booster showed good effectiveness in a couple of subgroups, as shown below, in this non-randomized study that had limited duration of follow-up for outcomes. It’s clearly a weaker study that the first 2 cited above that were in experimental models, but it’s real world, in people, and adds another line of support for the intranasal route for infection protection.
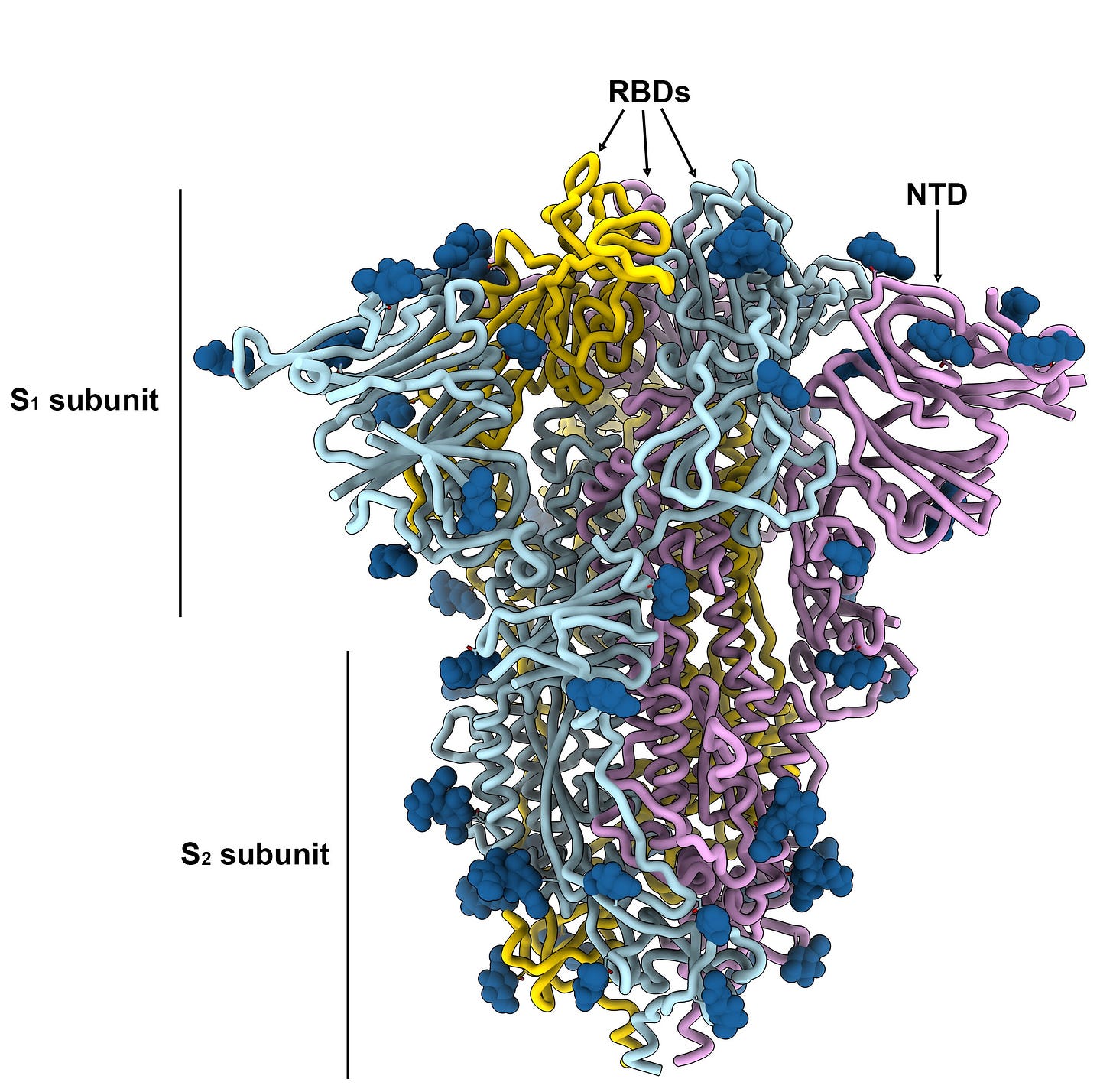
Although not a nasal or inhalation vaccine, this thread and preprint by David Veesler and team at University of Washington on the promise of a pan-coronavirus vaccine (directed against the conserved spike S2 subunit region) is quite encouraging. Like the receptor binding domain (RBD) or S2 subunit, these conserved regions of the spike would be worthy targets in the future, and, as noted above, the RBD was used in the dry powder inhalation vaccine.
Getting Covid
Recently, a colleague who I share an office with in clinic, and had the prior day, informed me that he had tested positive, was no longer a Novid. Early the next morning, I had a mild sore throat so I knew I’d finally been hit. I tested positive and started a prescription for Paxlovid soon thereafter. I had 2 days of marked fatigue, but was otherwise unaffected. Like most of you who have taken it, Paxlovid induced a bad metallic taste, but fortunately I didn’t experience other side effects. I tested negative for 2 days consecutively before ending isolation. While I normally exercise nearly every day, I put that on hold for 10 days. I had considered also taking metformin because of the randomized trial showing it can help prevent Long Covid, but there aren’t any data yet that have assessed the combination of paxlovid and metformin.
I consider myself extremely lucky compared with the experience of so many other friends, family members, colleagues and patients, particularly those at more advanced ages. Along the long course of the pandemic I had so many people write to me (or post on social media) about its inevitability and that I should just move on in life, stop masking, and don’t worry about it—”you’re not going to die.” I never agreed with that outlook, since we’ve made steady improvements throughout the pandemic in preventing severe Covid and Long Covid, such that the longer an infection can be delayed, the better. Of course, I’d much prefer to never have Covid, but there’s only so much one can do to prevent that from happening.
I had received the XBB.1.5 booster in late September, but still got infected 6-7 weeks later. That’s not at all surprising, since the booster doesn’t do much against infection, especially after the first month, and at peak might suppress infection by only 30-40%. But it does markedly amp up neutralizing antibodies (and T cell response) and certainly would be expected to help prevent severe Covid.
The experience exemplifies how much progress that we’ve made along the way. But there are still 2 absolutely vital objectives that haven’t been fulfilled: (1) highly effective treatments for Long Covid; and (2) inhalation vaccines to promote strong mucosal immunity and block infections and spread, effective against all variants. There’s still much work to do on both fronts, but I’m convinced we’ll eventually get there. If only we prioritized these like we did to get the initial Covid vaccines (think Operation Warp Speed), we’d likely be there by now.
Thanks for reading and subscribing to Ground Truths.
Wishing you and your family a happy holiday season,
Eric







Grateful for you, Eric Topol. Thank you for your work and for helping lay people understand complex issues, too.
Really appreciate your focus on long COVID, as so many millions of us are counting on this research to eventually restore our health. And thank you for sharing about your own recent experience with COVID. I’m glad you made it through okay and very smart to have waited before exercising.