Cancer and the Nervous System
An inextricable link that will lead to better treatments
Any type of connection, no less synapse, between cancer and the nervous system wasn’t something we heard about in medical school (←and still don’t). But in recent years there has been increasing attention to the importance of a bidirectional neural connects with cancer: the nervous system regulates the initiation and progression of cancer and cancer can hijack the nervous system. Both directions can lead to more proliferation and spread of tumors, no less neuronal dysfunction.
The field of “cancer neuroscience” has culminated in a brilliant new review article in this week’s Nature by Mancusi and Monje. It turns out there are multiple important types of crosstalk that occur between neurons and cancer cells.
Rich Crosstalk Between Neurons and Cancer Cells
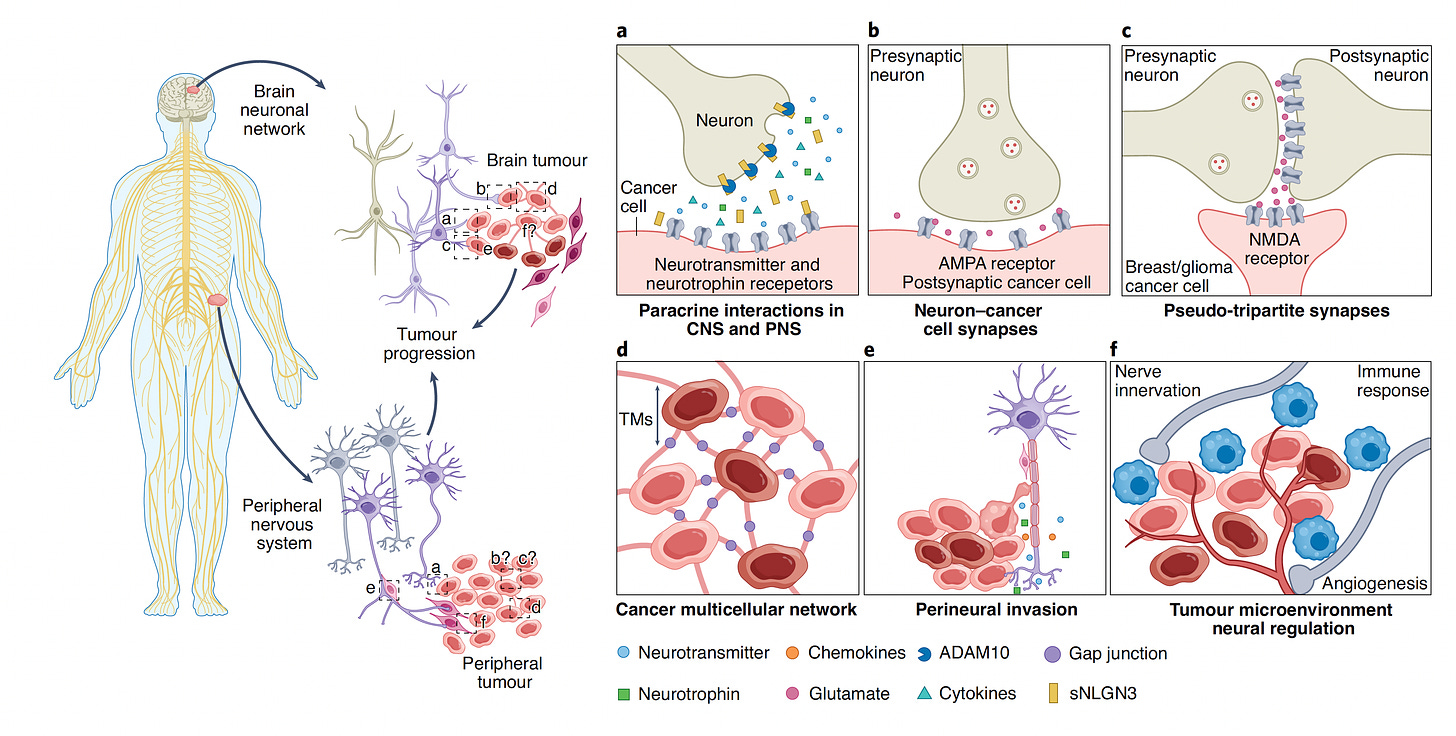
Stepping back from the review paper, a notable finding in 2019 was the direct synapse between a major type of brain tumors (glioma) and neurons, and how these synapses can drive progression of the cancer. Another distinct mechanism is from chemicals from nerve cells that release their transmitters (neurotransmitters, such as glutamate), neurotrophins, or other substances, as schematically shown by Pan and Winkler below. While these neurotransmitters and neurotrophins can directly promote cancer cell proliferation, there is also the potential of forming membrane tube connections (TMs), along with promoting multicellular cancer cell networks, cancer cell migration along the nerves (Panel e below) and influence on blood vessel formation and immune response (Panel f below). These processes can occur not just in the brain and spinal cord, but also in the peripheral nervous system throughout the body.
A few years ago in head and neck cancer it was found that p53 loss of function mutations, which are prominent across multiple cancer types, can lead to reprogramming of nerve cells to be adrenergic (capable of secreting epinephrine and norepinephrine neurotransmitters), which stimulates tumor progression. The schematic below shows that and introduces the concept of blocking these adrenergic transmitters in the experimental model to slow tumor proliferation.
There’s also much more to the immune response— a triangulated relationship between cancer, nerve and immune cells—as shown below (modified from Mancusi and Monte’s review paper)
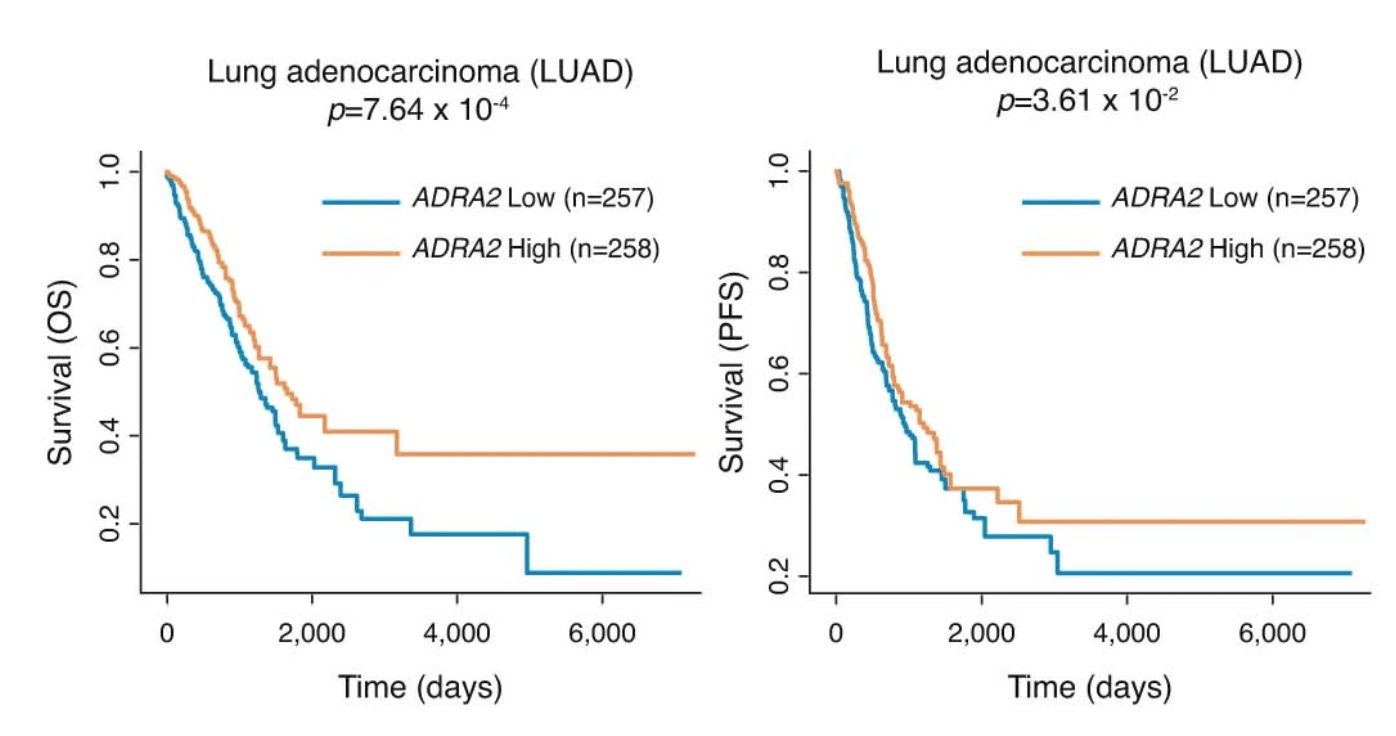
Bringing the immune cell function and adrenergic neurotransmitters together, a report just last week demonstrated [not p53 loss of function mutations] that promoting (agonists of) the α2-adrenergic receptor (medications such as clonidine, used for high blood pressure) improved the success of cancer immunotherapy in multiple tumor mouse models resistant to cancer immunotherapy and the authors concluded “our findings warrant the clinical testing of α2-adrenergic agonists (ADRA2 below) in patients with cancer.”
Some supportive evidence from patients with lung cancer was also presented that showed improved survival for those with high ADRA2 expression among 2 different cohorts.
This Science Magazine “dangerous partnership” diagram pulls together some of the mechanisms discussed above, and comes from a 2019 summary of many cancer-neuron crosstalk studies that have been seminal contributions to the field.
Broadly speaking, the convergence of cancer (and its therapy) with the nervous system is graphically depicted below.
The multi-dimensional connects between cancer and neurons has been demonstrated across many tumor types, including gastric, pancreatic, breast, basal cell, prostate and several others, much of which is reviewed in the new Nature paper.
The Mind and Cancer
Here in Ground Truths, I recently reviewed the fascinating study of patients with gliomas with surface brain electrical recordings and elegant biological profiles (see below) that showed the connection between the mind and cancer—talking or thinking was shown to promote tumor growth. Undoubtedly, factors such as stress have important interactions with cancer biology, and we’re likely to see these better understood in the future.
Emerging Treatments
Fortunately, all of these insights have been leading to many clinical trials, summarized in the Table below as of September 2022. Many startup companies have taken off to test interventions directed at the cancer-neuron axis.
The very recent state-of-the-science review by Winkler and colleagues in Cell nicely captures the many therapeutic opportunities at the intersection of cancer and neurons (see illustration below).
I really liked this summary statement in the Nature review: “Although targeting nervous system–cancer interactions may not by itself be sufficient to eradicate a tumor, this may be a necessary component of effective therapeutic regimens for currently intractable cancers such as high-grade gliomas and pancreatic cancers.”
The economist Robert Shiller wrote: “In the longer run and for wide-ranging issues, more creative solutions tend to come from imaginative interdisciplinary collaboration.” No question cancer fits the bill as an unmet and formidable challenge that can benefit from the groundwork of the studies reviewed here—by bringing together cancer biologists, neuroscientists, immunologists, cell biologists, and oncologists—to help advance the field. Hopefully, such trans-disciplinary collaboration can catalyze the cancer neuroscience field and shorten the requisite time that it took for cancer immunotherapy (at least 30 years) to be part of mainstream therapy.
Thanks for reading, sharing, and subscribing to Ground Truths!
Your free subscription denotes your support of this work. Should you decide to become a paid subscriber you should know that all proceeds go to support Scripps Research. That has already helped to bring on several of our summer high school and college interns.