The Big Miss: Inflammation and Cardiovascular Disease
The need for routine assessment and suppression of inflammation
We have known for many years that inflammation is a major driver of atherosclerosis and atherothrombosis (plaque + clot). There are now simple ways to measure body-wide inflammation, coronary artery inflammation, and many ways to reduce inflammation, including lifestyle modifications and inexpensive medications. But none of this has yet been incorporated in routine medical practice. In this issue of Ground Truths, I am going to review the body of evidence for taking inflammation seriously and what ought to amount to a rebooting of our approach to heart and vascular disease.
The Clinical Trials
Yesterday a new randomized trial of colchicine, a potent anti-inflammatory agent, to prevent events after stroke, was published in The Lancet. Over 3,100 patients with a non-severe, non-embolic stroke or TIA were randomly assigned to 0.5 mg colchicine per day plus usual care vs usual care only. The primary endpoint was the composite of heart attack, stroke, cardiac arrest, or hospitalization for unstable angina.
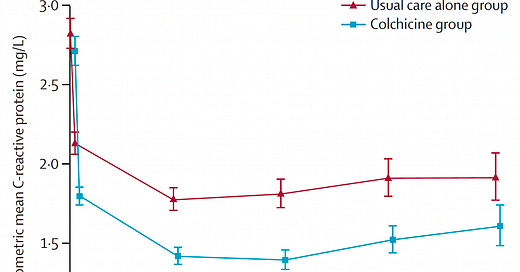
In the colchicine group, the event rate by intention-to-treat was 9.8% vs 11.7% in controls, a 16% reduction that was not statistically significant (upper bound 95% confidence interval 1.05). Colchicine led to a significant reduction of high sensitivity C-reactive protein (hs-CRP) at all time points assessed (Figure below). By a pre-specified on-treatment analysis, the primary endpoint was reduced from 11.7% to 8.0%, a 20% reduction, which was statically significant.
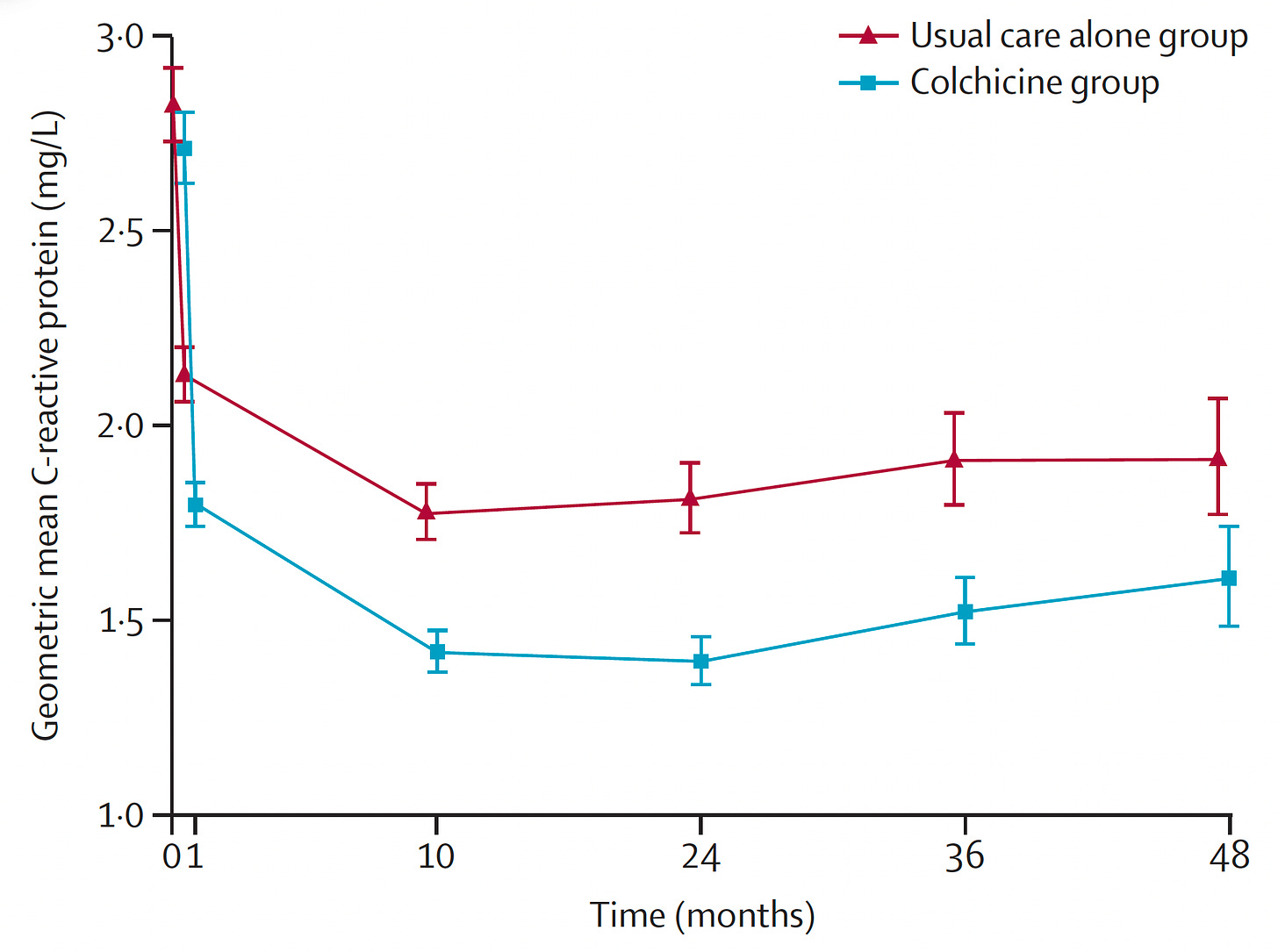
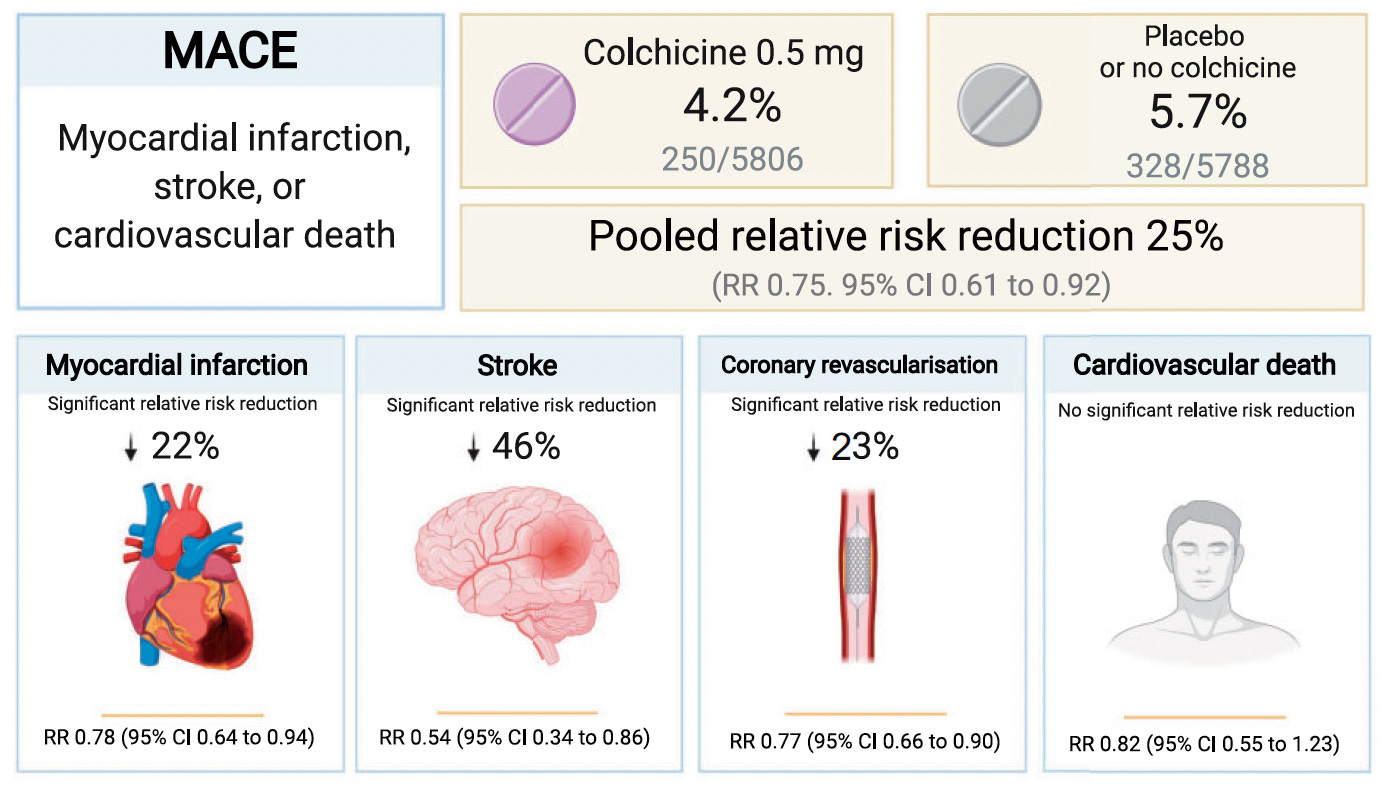
The new colchicine trial comes after 5 preceding ones that were subject to a meta- analysis. To summarize the 5 trials, the Table below shows 2 were large, each about 5,000 participants, one in chronic coronary artery disease and the other after heart attack, both with about 2-year follow-up.
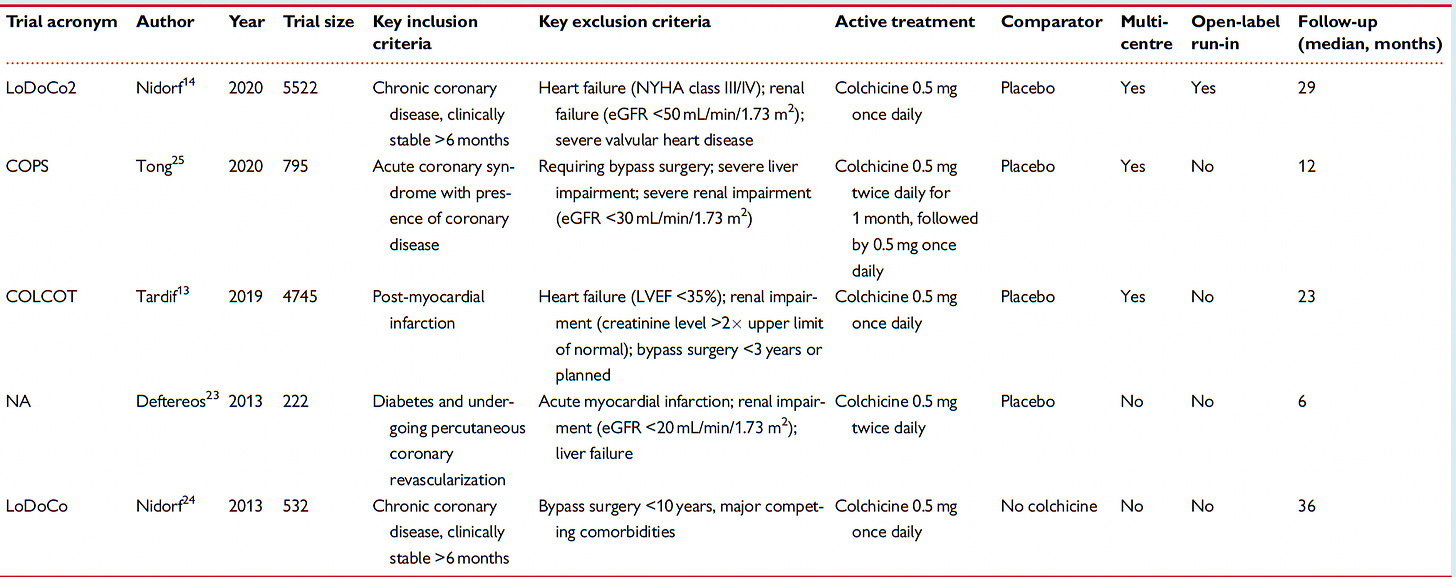
There was a very consistent reduction of heart attack, stroke and coronary revascularization, as seen below. While some of the trials noted increased in infection requiring hospitalization or pneumonia, this adverse effect was not statistically significant in aggregate. Nor was a reduction in cardiovascular death.
This simplified graphic summarizes that meta-analysis.
The FDA approved colchicine (LoDoCo) in June 2023 for reducing cardiovascular events, the first anti-inflammatory agent for this indication. Had a Bayesian analysis been applied to the new stroke trial, it would certainly have achieved statistical significance, since the results are well aligned with the previous 5 trials.
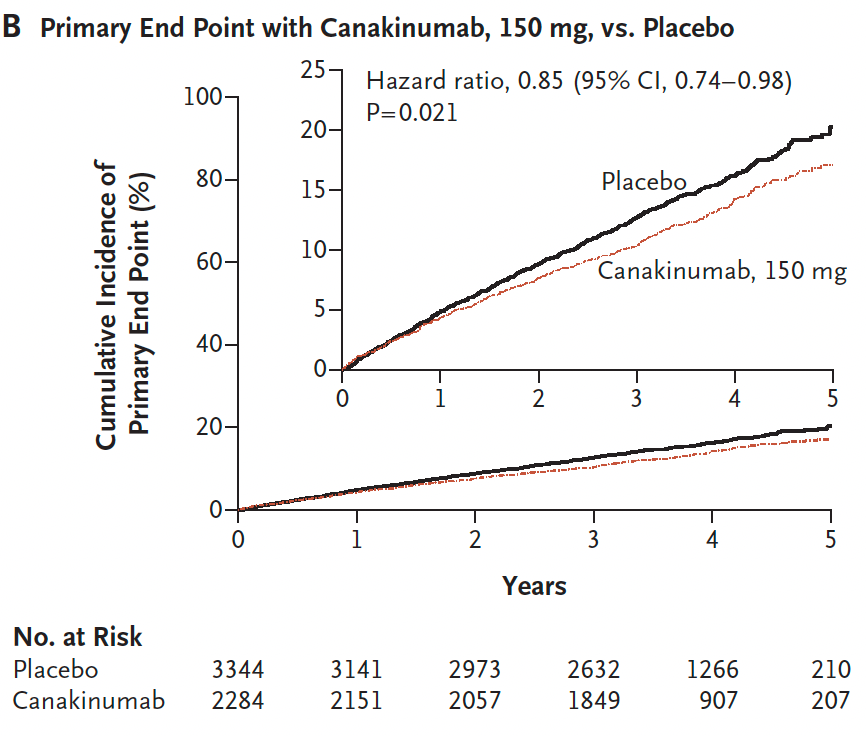
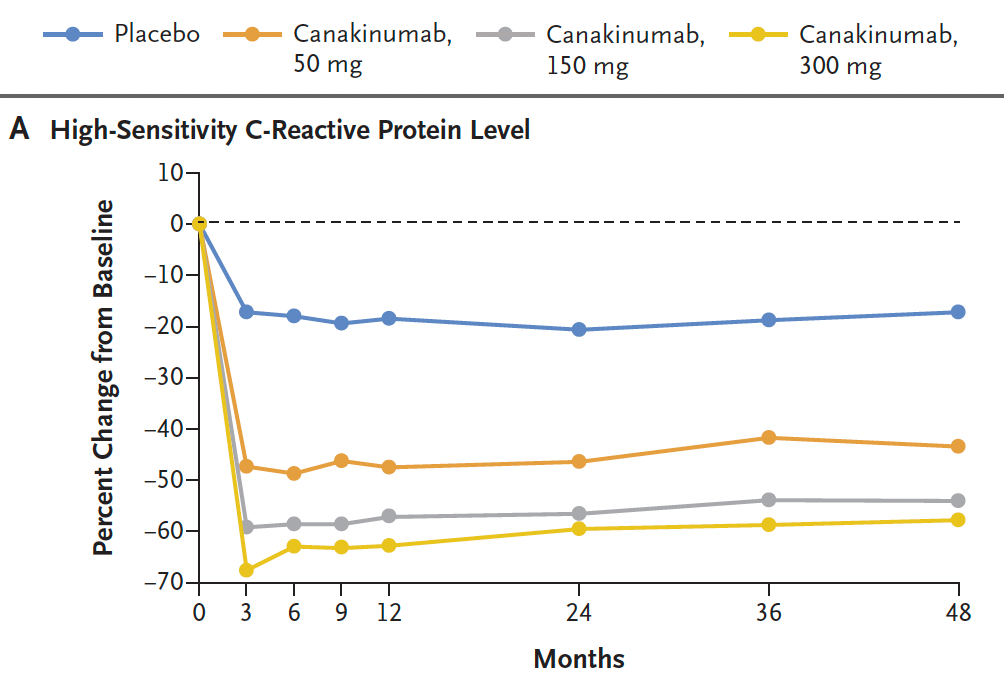
The anti-inflammatory story goes beyond colchicine. Back in 2017, a large trial known as CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study) tested a monoclonal antibody (3 different doses, given at 3-month intervals) to interleukin-1β vs placebo in over 10,000 patients with a prior heart attack and hs-CRP of 2 mg/l or greater. The 2 higher drug doses led to about 15% reduction of the primary endpoint of heart attack, stroke or cardiovascular death. The 150 mg dose results are shown below, the 300 mg dose was similar in effect. The 3 doses combined was statistically significant for reducing the primary endpoint. The absolute event rates were presented by incidence rate per 100 person-years, which is not what I would like to see (ugh, present absolute events, please) and were reduced from 4.5 to 3.9 in the two high dose groups. The reduction of the primary endpoint was achieved without any change in lipids. Note this point because all of our attention these days is focused on lipid lowering for addressing arterial inflammation. There are other. complementary ways to do this!
There was a dose-response reduction hs-CRP as shown below
The drawback in this trial was a higher rate of fatal infection with the treatment: 0.18% in the control group vs 0.30% in the 2 higher dose groups of drug. It’s a small absolute difference of about 12 per 10,000 people, but nonetheless a serious adverse effect reflecting suppression of the immune response to an infection. The company developing this drug, Novartis, decided not to pursue the cardiovascular indication.
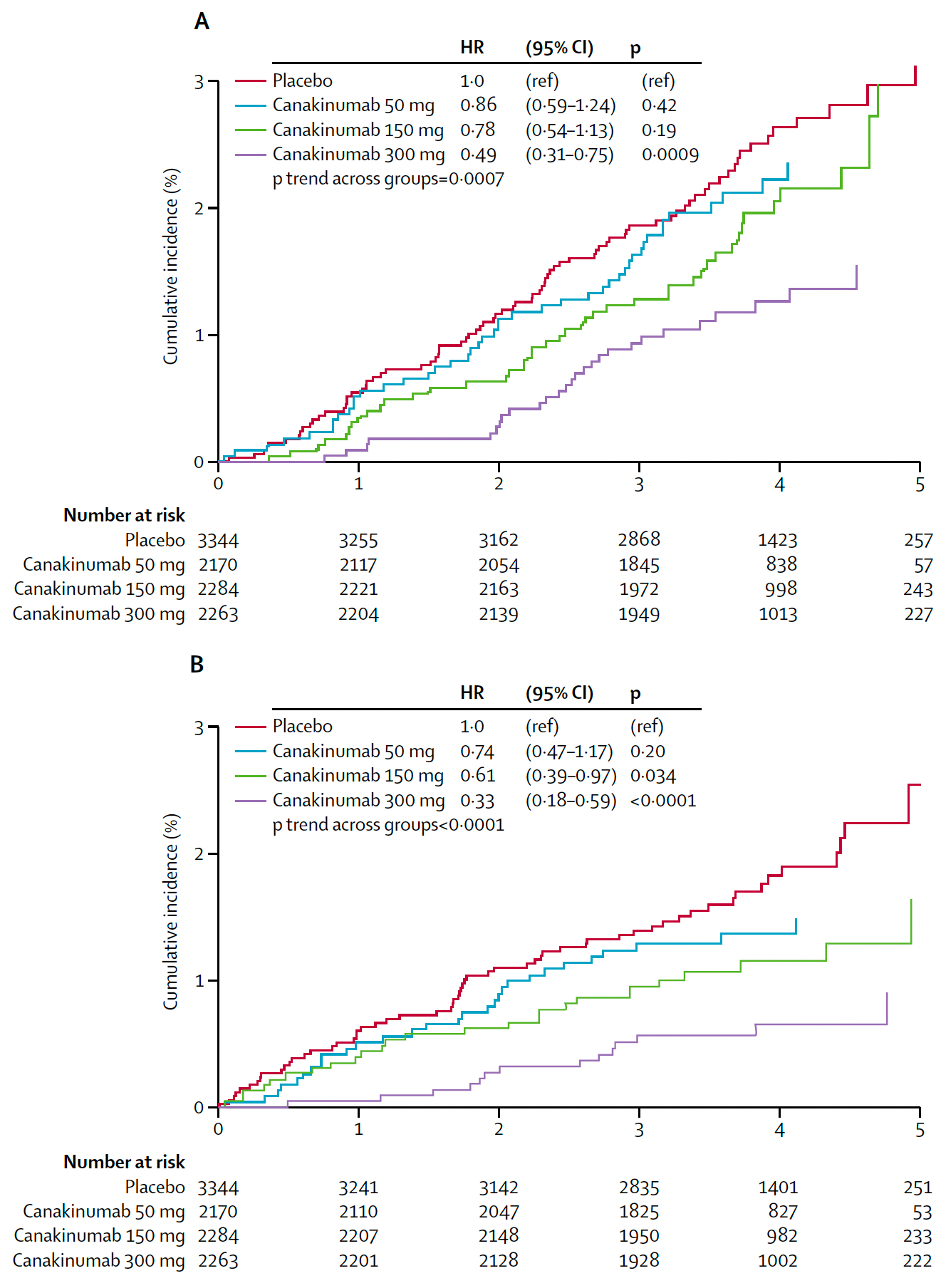
Of note, and perhaps not surprising in retrospect, in view of the common underpinning of chronic inflammation, was the significant dose-response effect the drug had for reducing fatal cancer and lung cancer in a heart disease trial. A twofer!
(Top graph is for fatal cancer, Bottom is lung cancer)
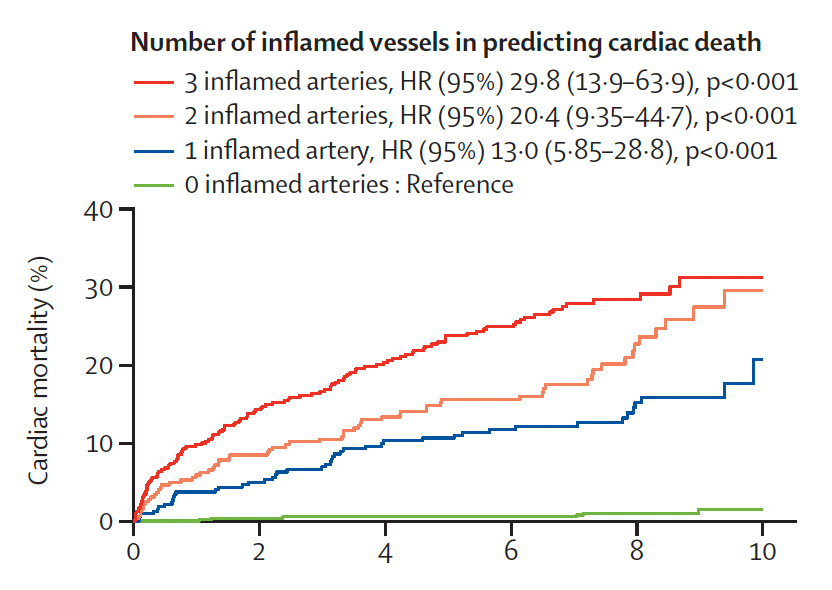
Detection of Inflammation
Besides the blood marker hs-CRP which costs less than $30, a new, large study using CT coronary angiograms (CCTA) shed light on another means that is more direct. The fat surrounding each of the 3 coronary arteries (a fat attenuation index, FAI) can be used to determine the presence or absence of inflammation). There was a striking relationship between coronary artery inflammation and adverse outcomes. Overall there were CCTAs among over 40,000 consecutive patients in 8 UK hospitals followed for 2.7 years for heart attack, heart failure of cardiac death). 81% had non-obstructive coronary disease by the CT scan. but accounted for over 64% of MACE and cardiac deaths. A subset of 3,393 patients had long term 7.7 year follow-up. For the latter group, below is the plot of number of inflamed arteries vs cardiac death. Note it is a whopping 30-fold for all 3 arteries inflamed, and 13-fold for one-artery.
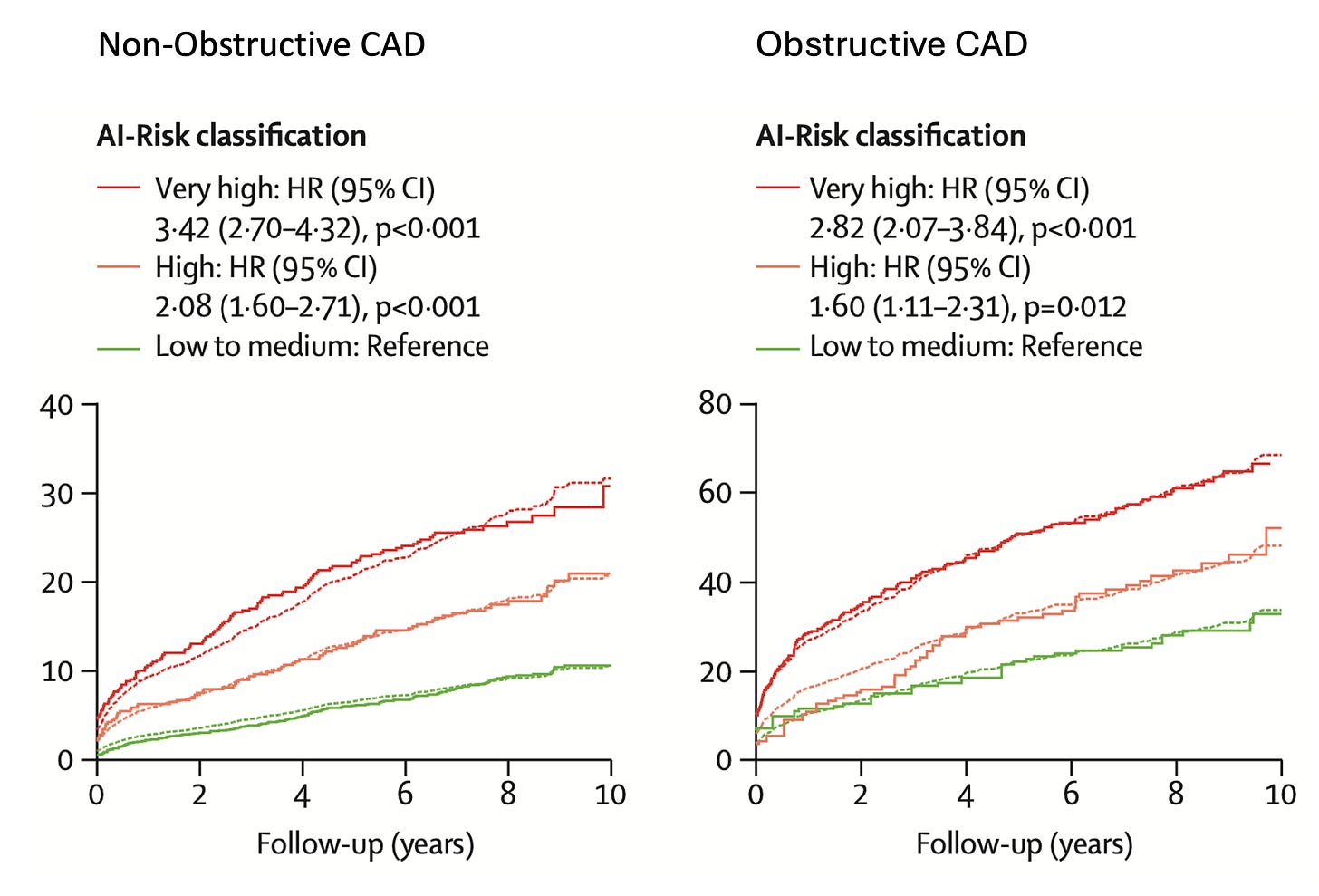
The AI-risk score, which integrated the coronary inflammation data and clinical features, was assessed for patients with and without obstructive coronary disease. As seen below, the non-obstructive group had about half of MACE events as the obstructive (note the different Y-axes), but the AI-risk score differentiated both groups well.
There are still some technical uncertainties for using the FAI clinically, such as reproducibility across centers, but these results provide new insight to the prognostic value of inflammation in a clinical world that is obstruction-centric. The FAI is not generally provided for CCTAs that are performed today.
Vulnerable Plaque
Using intra-arterial imaging during coronary angiography, fatty, thin-capped, vulnerable plaque that does not limit blood flow can be identified and these correlate with an increase risk of MACE. A recent randomized trial compared intervention (mostly stenting in 90%) vs medical therapy for 1606 patients with vulnerable plaque. At 2 year follow-up the primary outcome (death, target vessel heart attack or revascularization) occurred in 3.4% of the medical therapy group compared with 0.4% in. the intervention group, a significant 46% reduction (P=0.003). These results tell us once again that detecting inflammation via coronary imaging can lead to a lower number of adverse events. Just as colchicine was the first drug approved for anti-inflammation in cardiovascular disease, so this was the first trial to show benefit of treating vulnerable plaques. I wonder how people with such vulnerable plaque would do with an effective anti-inflammatory drug.
Where to Go From Here
The totality of these findings highlight the importance of systemic and arterial inflammation for risk of major adverse cardiovascular events. We should be using biomarkers, such as hs-CRP, and building on that with better ones that provide an index for body-wide inflammation. We have a cheap drug that has proven efficacy in 6 randomized trials—colchicine. It’s hardly used by cardiologists or physicians in general to reduce risk. The proprietary form of the drug (LoDoCo) is 0.5 mg (once per day) as assessed in the trials, but the generic 0.6 mg, which should have the same effect, is less than 1/20th of the price (GoodRx $300 vs $15). The problem with colchicine is that it frequently induces gastrointestinal side effects, particularly diarrhea, in about 1 in 4 people. We clearly need better anti-inflammatory agents with higher efficacy and less side effects. But little work is being done to pursue this goal.
The big miss is that we continue to be focused only on lipid lowering and flow-limiting atherosclerotic narrowings, without adequate attention to detecting inflammation, using anti-inflammatory agents (that are not lipid directed), and acknowledging the adverse prognostic potential of non-obstructive arterial disease. The evidence has mounted to change course and adapt a broader view that will help reduce major adverse cardiovascular events in people at-risk.
****************************************
I’m appreciative of your reading and subscribing to Ground Truths. Even more, please share the post if you think it’s informative.
These newsletters and the podcasts are provided free, open-access. Voluntary paid subscriptions all go to support Scripps Research. Many thanks for that—they greatly helped fund our summer internship programs for 2023 and 2024.


Thanks for this. Wondering what relationship/benefit you think this may have in post-COVID hyper inflammatory conditions?
Excellent, thank you for this post Dr. Topol!