Why We Need an Immunome
How can we know the primacy of our immune response for health yet be unable to measure it?
It is startling that here we are in 2024, recognizing how critical our immune system is for protecting us against infections and major diseases, such as cancer, and how it tells us about our aging process (immunosenescence), yet we have no informative clinical test to get at it.
The crude way we can assess our immune system is from a complete blood count (CBC) looking at the white blood cell (neutrophil) to lymphocyte ratio (NLR). It is a very rough assessment of the balance between inflammation (neutrophil count) vs immune system (lymphocyte count) and is associated with a poor prognosis for cancer, higher risk of major cardiovascular events, infection, and all-cause mortality. The associations are statistically supported but of little help for interpretation at the individual level. Accordingly, most clinicians don’t even look at it.
Back in 2015, I was excited about a report in Science on VIrScan. A drop of blood detecting antibodies— to >1,000 virus strains from over 200 species—could tell us about every virus a person has been exposed to and when for as little as $25! A sample of output for 14 virus strains is shown below
While this isn’t by any means an immunome that would tell us about the critical components of our immune response and predict outcomes, it was certainly a big step in the right direction. Now, nearly a decade later, I wondered what happened to the VirScan. Yesterday, I contacted Stephen Elledge, the senior author of this paper, and he let me know that it would soon be available through Infinity Bio, But it’s unclear whether, when and how this test will be part of clinical care. And it certainly won’t be for $25!
Throughout the Covid pandemic we’ve seen the importance of T cells—helper CD4+ and cytotoxic CD8+—from research studies, telling us about our immune response to the virus, its many variants, and vaccines. But none of these T cells tests are commercially available. They’re only done in research labs.
Now let’s review 4 studies that assessed the immune system and clinical outcomes.
IMM-AGE
One of the first attempts to come up with an immunome—correlating a composite of immune system markers and clinical outcomes—was in 135 healthy individuals followed for 9 years. The immune system profile included T and B cells, NK cells, cytokine production, and gene expression. It didn’t include antibody or interferon assessment. As might be anticipated, there was considerable inter-individual variability but overall the profile correlated well with chronological age. It turned out to be quite informative.
An IMM-AGE score based on the profile, applied to Framingham Heart Study Offspring participants. was associated with all-cause mortality during follow-up. It also was better than DNA methylation (epigenetic) clocks for predicting mortality.
iAge
The iAge was derived from deep learning A.I. of circulating blood markers from 1,001 participants aged 8 to 96 years, including 50 cytokines, chemokines and growth factors, gene expression, immune cell phenotypes and counts (such as CD4+, CD8+, B cells), and cytomegalovirus (CMV) exposure.
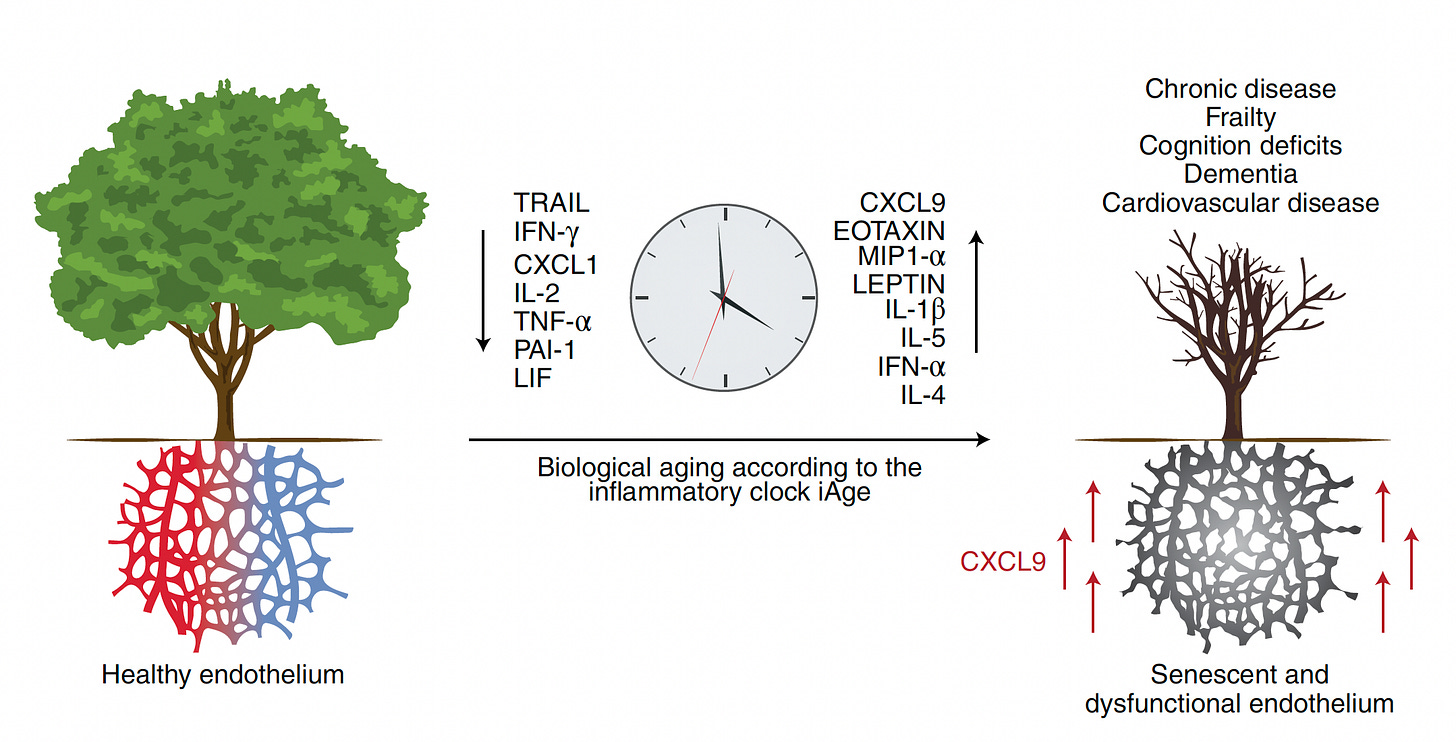
Indeed, iAge correlated with chronological age (0.78) and number of comorbidities; the protective iAge index (chronological age minus rank iAge), as seen below, with centenarians exhibiting an advantage compared with younger individuals (small N, 19 vs 18, respectively). Beyond that, iAge correlated with frailty, chronic diseases, cognitive decline and cardiovascular aging, as well as IMM-AGE. A major factor that contributed to iAge’s predictive capacity was CXCL9, which is induced by interferon-gamma and attracts T cells.
By studying aged endothelial cells and differentiating induced pluripotent stem cells into endothelial cells, CXCL9 was identified as a master regulator of blood vessel function and cell aging, as schematically (and simplified) shown below. Silencing CXCL9 reversed these age-related endothelial changes.
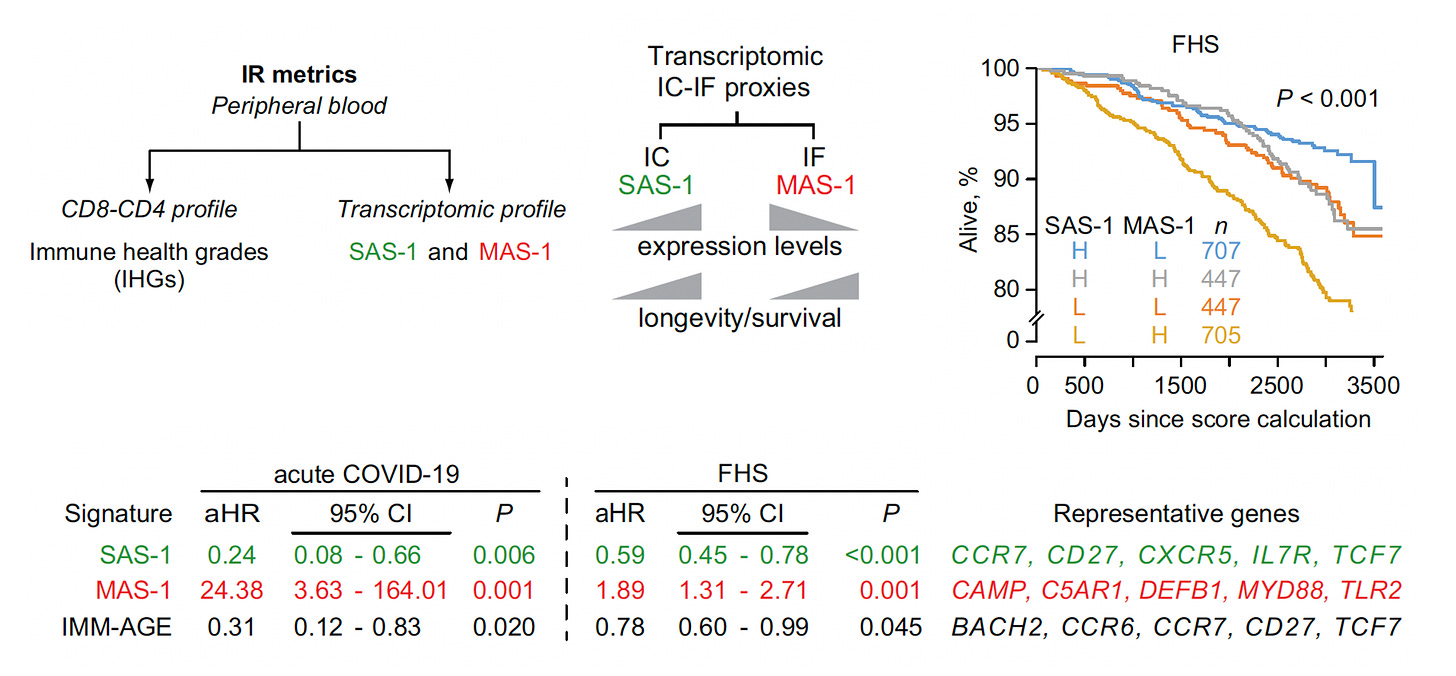
Immune Health Grade and Immune Resilience
A study that assessed CD4+ and CD8+ cells (immune health grade) and gene expression (transcriptomics) to get at the balance of immunocompetence (IC) and inflammation (IF) for quantifying immune resilience. Think of it as major refinement beyond the neutrophil to lymphocyte ratio. As seen below, high SAS-1 (gene expression linked with immunocompetence) and low MAS-1 (gene expression linked with inflammation), was associated with best survival over 10 years in the Framingham Heart Study (FHS).
Immune Health Metric (IHM)
Published this month was a study of 228 participants with various genetic immune conditions, along with age and sex-matched healthy controls, with A.I. to derive a score. The immune profiling included complete blood count with B cells, T cells, NK cells, platelets, transcriptomics, proteins, with modules of the RNA and protein data.
The IHM was assessed in 10 independent datasets and differentiated healthy vs immunologic or inflammatory diseases, with discrimination well beyond inflammatory markers such as C-reactive protein and interleukin-6. It also predicted age among healthy individuals, and the age-related response to vaccines. The IHM’s predictive capacity was not affected by removal of CXCL9 (iAge) but it was concordant with IMM-AGE.
Specific Components
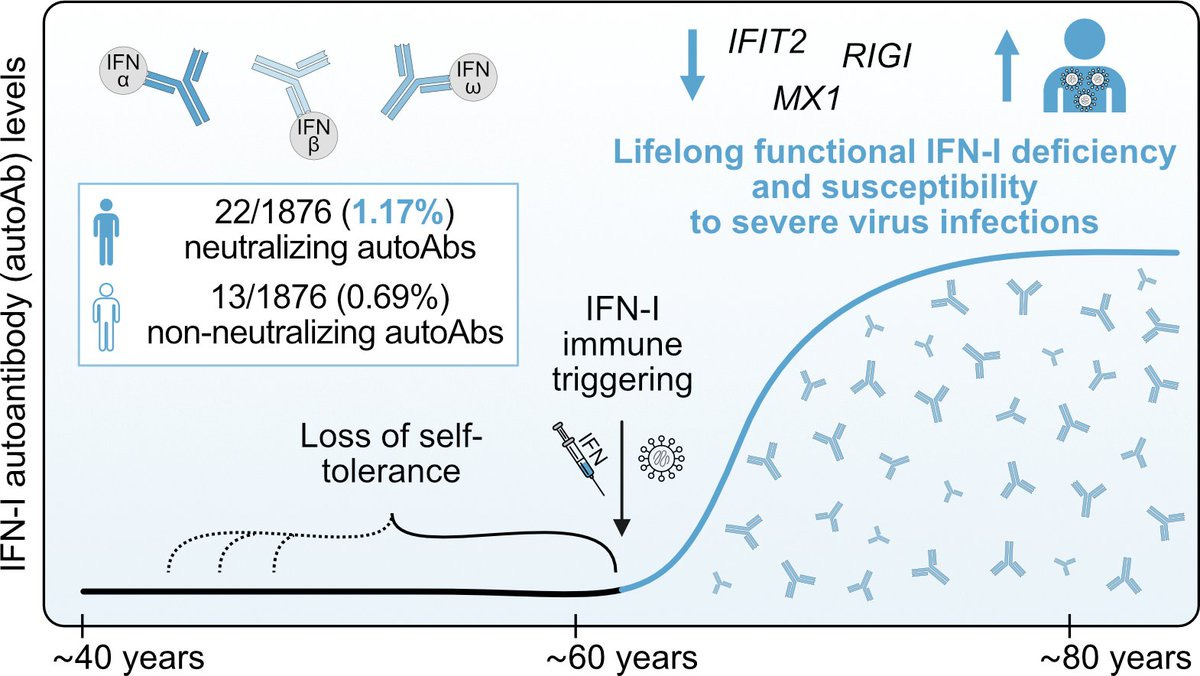
This past week it was reported that about 2% of people aged 60 years and beyond develop anti-interferon-1 (IFN-1) antibodies that are persistent and linked to vulnerability to severe illness from viral infections.
Where to Go From Here?
With a large body of knowledge indicating the immune system as a (if not the) major determinant for our health and diseases, we desperately need a means for assessing our immune system. It could predict a person’s response to infections, vulnerability to cancer or its spread, no less cardiovascular and neurodegenerative disease susceptibility. Since our immune system function is quite variable with aging, knowing a person of advanced age is not immunocompetent could lead to ways to augment the immune response. There are diverse means that could be accomplished in the future, such as via the gut microbiome through pre- or probiotics. Or vaccines. Even lifestyle factors such as diet, exercise and sleep are actionable modulators of our immune response.
Perhaps the most striking impact of the immune response relates to treatment for cancer. We have seen notable progress with immune checkpoint inhibitors, but that is often transient, and bolstered with many other strategies to rev up the immune system including CAR T therapy, bispecific T cell engagers (BiTES), cell-drug conjugates, JAK-kinase inhibitors, tumor infiltrating lymphocytes, and neoantigen cancer vaccines. All of these options, and their combinations, are targeting the patient’s immune response to the tumor, but none are directed to the health of their immune system per se. We’re “throwing the book” of immunotherapy treatments and increasing success, but ironically we’re not able to measure the patient’s intrinsic immune system’s status.
For Long Covid, an immunome could help—at the individual level— unravel this devastating condition’s underlying pathophysiology, which in many affected people involves a dysregulated immune response or an autoimmune component (or both). That could guide us to an effective treatment, which is now lacking.
Sure the immune system is complex with interferons, antibodies, innate and adaptive immunity. But high-throughput assays of proteins, antibodies, cell phenotyping, micro- and nanofluidics, no less A.I. analytics, makes this eminently possible now. Developing a practical, inexpensive immunome is an imperative to testing such ideas and we have none. Just multiple impressive research studies dangling summarized here, all independently reinforcing its potential value. The same vacuous state applies to the related inflammation biomarkers with only primitive ones such as C-reactive protein available, and not conventionally used (see my prior Ground Truths posts on protein clocks or the big miss).
Unfortunately, diagnostic tests do not get the same priority in medicine as therapeutics, both by the life science industry and regulatory oversight/streamlining.
I hope I have convinced you that having an immunome is an important part of the future of medicine and hope that we’ll get there someday. We should accelerate our efforts to get there and build on the promising studies I’ve reviewed.
Thanks for reading and subscribing to Ground Truths.
If you found this post interesting or provocative please share with your colleagues and network.
These newsletters and the podcasts are provided free, open-access, without ads. Voluntary paid subscriptions all go to support Scripps Research. Many thanks for that—they greatly helped fund our summer internship programs for 2023 and 2024.






As a chronic lymphocytic leukemia patient who has been through a clinical trial that included a long lasting immunosuppressive therapy, I think Digital Twins work is quite applicable here in narrowing down metrics and validating them:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10873299/
Forum on immune digital twins: a meeting report
NPJ Syst Biol Appl. 2024; 10: 19.
There are several YouTubes of this conference for more detail, as well.
IgRT (Immunoglobulin Replacement Therapies) such as IVIG (IntraVenous ImmunoGlobulin) and SCIG (SubCutaneous ImmunoGlobulin) are insanely expensive (>US $15K/month). Infections can lead to even more expensive hospitalizations. Identifying the most at risk of infection would be really helpful here. But all we have to go on is a century-old blood count and a more recent IgG count. Many patients do just fine despite low levels of neutrophils and IgG, while others get pneumonias despite normal levels.
During the pandemic, I did Adpative Biotechnologies T-Detect, a qualitative TCR (T-cell Receptor) massive sequencing test. It has not become a product, however. As part of my leukemia trial, I did Adaptive Biotechnologies ClonoSEQ massive BCR (B-cell Receptor) test to track my CLL clones. It also reports on unique BCR clones, which I find useful in observing B-cell recovery from therapy. Their sequencing technology and databses could be very useful in epitope and risk analysis at the patient level.
Finally, I'd like to put in a vote for cytokine blood panel studies. Even though many infections are local, with a corresponding local cytokine population. there are systemic effects as well that may answer ancient questions about additional symptoms such as fatique, body aches, and headaches.