Funding for the NIH and US biomedical research is imperiled at a momentous time of progress. Exemplifying this is the work of Dr. Anna Greka, a leading physician-scientist at the Broad Institute who is devoted to unlocking the mysteries of rare diseases— that cumulatively affect 30 million Americans— and finding cures, science supported by the NIH.
A clip from our conversation
The audio is available on iTunes and Spotify. The full video is linked here, at the top, and also can be found on YouTube.
Transcript with audio and external links
Eric Topol (00:06):
Well, hello. This is Eric Topol from Ground Truths, and I am really delighted to welcome today, Anna Greka. Anna is the president of the American Society for Clinical Investigation (ASCI) this year, a very prestigious organization, but she's also at Mass General Brigham, a nephrologist, a cell biologist, a physician-scientist, a Core Institute Member of the Broad Institute of MIT and Harvard, and serves as a member of the institute’s Executive Leadership Team. So we got a lot to talk about of all these different things you do. You must be pretty darn unique, Anna, because I don't know any cell biologists, nephrologists, physician-scientist like you.
Anna Greka (00:48):
Oh, thank you. It's a great honor to be here and glad to chat with you, Eric.
Eric Topol (00:54):
Yeah. Well, I had the real pleasure to hear you speak at a November conference, the AI for Science Forum, which we'll link to your panel. Where I was in a different panel, but you spoke about your extraordinary work and it became clear that we need to get you on Ground Truths, so you can tell your story to everybody. So I thought rather than kind of going back from the past where you were in Greece and somehow migrated to Boston and all that. We're going to get to that, but you gave an amazing TED Talk and it really encapsulated one of the many phenomenal stories of your work as a molecular sleuth. So maybe if you could give us a synopsis, and of course we'll link to that so people could watch the whole talk. But I think that Mucin-1 or MUC1, as you call it, discovery is really important to kind of ground our discussion.
A Mysterious Kidney Disease Unraveled
Anna Greka (01:59):
Oh, absolutely. Yeah, it's an interesting story. In some ways, in my TED Talk, I highlight one of the important families of this story, a family from Utah, but there's also other important families that are also part of the story. And this is also what I spoke about in London when we were together, and this is really sort of a medical mystery that initially started on the Mediterranean island of Cyprus, where it was found that there were many families in which in every generation, several members suffered and ultimately died from what at the time was a mysterious kidney disease. This was more than 30 years ago, and it was clear that there was something genetic going on, but it was impossible to identify the gene. And then even with the advent of Next-Gen sequencing, this is what's so interesting about this story, it was still hard to find the gene, which is a little surprising.
Anna Greka (02:51):
After we were able to sequence families and identify monogenic mutations pretty readily, this was still very resistant. And then it actually took the firepower of the Broad Institute, and it's actually from a scientific perspective, an interesting story because they had to dust off the old-fashioned Sanger sequencing in order to get this done. But they were ultimately able to identify this mutation in a VNTR region of the MUC1 gene. The Mucin-1 gene, which I call a dark corner of the human genome, it was really, it's highly repetitive, very GC-rich. So it becomes very difficult to sequence through there with Next-Gen sequencing. And so, ultimately the mutation of course was found and it's a single cytosine insertion in a stretch of cytosines that sort of causes this frameshift mutation and an early stop codon that essentially results in a neoprotein like a toxic, what I call a mangled protein that sort of accumulates inside the kidney cells.
Anna Greka (03:55):
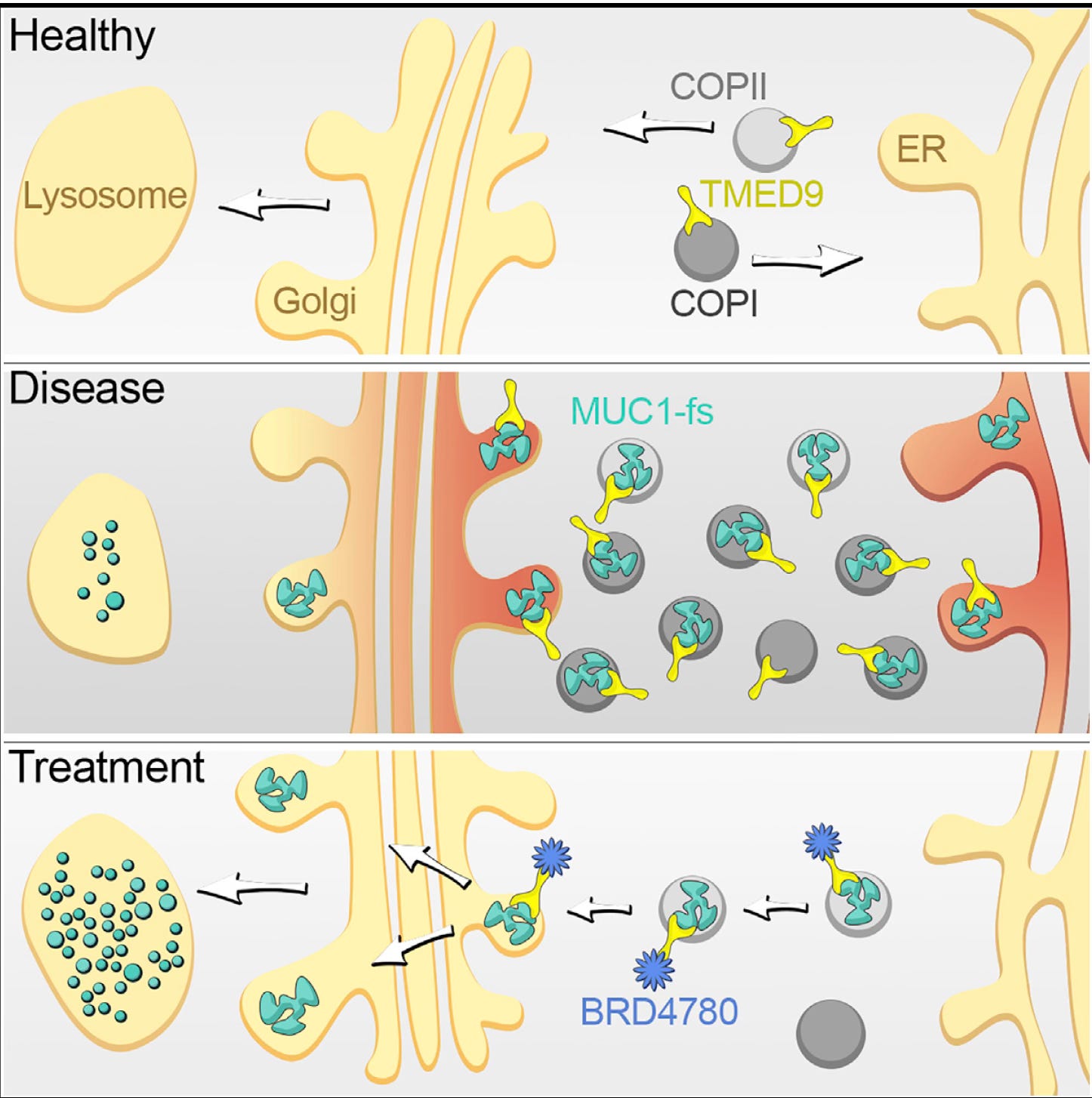
And that's where my sort of adventure began. It was Eric Lander’s group, who is the founding director of the Broad who discovered the mutation. And then through a conversation we had here in Boston, we sort of discovered that there was an opportunity to collaborate and so that’s how I came to the Broad, and that's the beginnings of this story. I think what's fascinating about this story though, that starts in a remote Mediterranean island and then turns out to be a disease that you can find in every continent all over the world. There are probably millions of patients with kidney disease in whom we haven't recognized the existence of this mutation. What's really interesting about it though is that what we discovered is that the mangled protein that's a result of this misspelling of this mutation is ultimately captured by a family of cargo receptors, they’re called the TMED cargo receptors and they end up sort of grabbing these misfolded proteins and holding onto them so tight that it's impossible for the cell to get rid of them.
Anna Greka (04:55):
And they become this growing heap of molecular trash, if you will, that becomes really hard to manage, and the cells ultimately die. So in the process of doing this molecular sleuthing, as I call it, we actually also identified a small molecule that actually disrupts these cargo receptors. And as I described in my TED Talk, it's a little bit like having these cargo trucks that ultimately need to go into the lysosome, the cells recycling facility. And this is exactly what this small molecule can do. And so, it was just like a remarkable story of discovery. And then I think the most exciting of all is that these cargo receptors turn out to be not only relevant to this one mangled misshapen protein, but they actually handle a completely different misshapen protein caused by a different genetic mutation in the eye, causing retinitis pigmentosa, a form of blindness, familial blindness. We're now studying familial Alzheimer's disease that's also involving these cargo receptors, and there are other mangled misshapen proteins in the liver, in the lung that we're now studying. So this becomes what I call a node, like a nodal mechanism that can be targeted for the benefit of many more patients than we had previously thought possible, which has been I think, the most satisfying part about this story of molecular sleuthing.
Eric Topol (06:20):
Yeah, and it's pretty extraordinary. We'll put the figure from your classic Cell paper in 2019, where you have a small molecule that targets the cargo receptor called TMED9.
Anna Greka (06:34):
Correct.
Expanding the Mission
Eric Topol (06:34):
And what's amazing about this, of course, is the potential to reverse this toxic protein disease. And as you say, it may have applicability well beyond this MUC1 kidney story, but rather eye disease with retinitis pigmentosa and the familial Alzheimer's and who knows what else. And what's also fascinating about this is how, as you said, there were these limited number of families with the kidney disease and then you found another one, uromodulin. So there's now, as you say, thousands of families, and that gets me to part of your sleuth work is not just hardcore science. You started an entity called the Ladders to Cures (L2C) Scientific Accelerator.
Eric Topol (07:27):
Maybe you can tell us about that because this is really pulling together all the forces, which includes the patient advocacy groups, and how are we going to move forward like this?
Anna Greka (07:39):
Absolutely. I think the goal of the Ladders to Cures Accelerator, which is a new initiative that we started at the Broad, but it really encompasses many colleagues across Boston. And now increasingly it's becoming sort of a national, we even have some international collaborations, and it's only two years that it's been in existence, so we're certainly in a growth mode. But the inspiration was really some of this molecular sleuthing work where I basically thought, well, for starters, it cannot be that there's only one molecular node, these TMED cargo receptors that we discovered there's got to be more, right? And so, there's a need to systematically go and find more nodes because obviously as anyone who works in rare genetic diseases will tell you, the problem for all of us is that we do what I call hand to hand combat. We start with the disease with one mutation, and we try to uncover the mechanism and then try to develop therapies, and that's wonderful.
Anna Greka (08:33):
But of course, it's slow, right? And if we consider the fact that there are 30 million patients in the United States in every state, everywhere in the country who suffer from a rare genetic disease, most of them, more than half of them are children, then we can appreciate the magnitude of the problem. Out of more than 8,000 genes that are involved in rare genetic diseases, we barely have something that looks like a therapy for maybe 500 of them. So there's a huge mismatch in the unmet need and magnitude of the problem. So the Ladders to Cures Accelerator is here to address this and to do this with the most modern tools available. And to your point, Eric, to bring patients along, not just as the recipients of whatever we discover, but also as partners in the research enterprise because it's really important to bring their perspectives and of course their partnerships in things like developing appropriate biomarkers, for example, for what we do down the road.
Anna Greka (09:35):
But from a fundamental scientific perspective, this is basically a project that aims to identify every opportunity for nodes, underlying all rare genetic diseases as quickly as possible. And this was one of the reasons I was there at the AI for Science Forum, because of course when one undertakes a project in which you're basically, this is what we're trying to do in the Ladders to Cures Accelerator, introduce dozens of thousands of missense and nonsense human mutations that cause genetic diseases, simultaneously introduce them into multiple human cells and then use modern scalable technology tools. Things like CRISPR screens, massively parallel CRISPR screens to try to interrogate all of these diseases in parallel, identify the nodes, and then develop of course therapeutic programs based on the discovery of these nodes. This is a massive data generation project that is much needed and in addition to the fact that it will help hopefully accelerate our approach to all rare diseases, genetic diseases. It is also a highly controlled cell perturbation dataset that will require the most modern tools in AI, not only to extract the data and understand the data of this dataset, but also because this, again, an extremely controlled, well controlled cell perturbation dataset can be used to train models, train AI models, so that in the future, and I hope this doesn't sound too futuristic, but I think that we're all aiming for that cell biologists for sure dream of this moment, I think when we can actually have in silico the opportunity to make predictions about what cell behaviors are going to look like based on a new perturbation that was not in the training set. So an experiment that hasn't yet been done on a cell, a perturbation that has not been made on a human cell, what if like a new drug, for example, or a new kind of perturbation, a new chemical perturbation, how would it affect the behavior of the cell? Can we make a predictive model for that? This doesn't exist today, but I think this is something, the cell prediction model is a big question for biology for the future. And so, I'm very energized by the opportunity to both address this problem of rare monogenic diseases that remains an unmet need and help as many patients as possible while at the same time advancing biology as much as we possibly can. So it's kind of like a win-win lifting all boats type of enterprise, hopefully.
Eric Topol (12:11):
Yeah. Well, there's many things to get to unpack what you've just been reviewing. So one thing for sure is that of these 8,000 monogenic diseases, they have relevance to the polygenic common diseases, of course. And then also the fact that the patient family advocates, they are great at scouring the world internet, finding more people, bringing together communities for each of these, as you point out aptly, these rare diseases cumulatively are high, very high proportion, 10% of Americans or more. So they're not so rare when you think about the overall.
Anna Greka (12:52):
Collectively.
Help From the Virtual Cell?
Eric Topol (12:53):
Yeah. Now, and of course is this toxic proteinopathies, there's at least 50 of these and the point that people have been thinking until now that, oh, we found a mangled protein, but what you've zeroed in on is that, hey, you know what, it's not just a mangled protein, it's how it gets stuck in the cell and that it can't get to the lysosome to get rid of it, there's no waste system. And so, this is such fundamental work. Now that gets me to the virtual cell story, kind of what you're getting into. I just had a conversation with Charlotte Bunne and Steve Quake who published a paper in December on the virtual cell, and of course that's many years off, but of course it's a big, bold, ambitious project to be able to say, as you just summarized, if you had cells in silico and you could do perturbations in silico, and of course they were validated by actual experiments or bidirectionally the experiments, the real ones helped to validate the virtual cell, but then you could get a true acceleration of your understanding of cell biology, your field of course.
Anna Greka (14:09):
Exactly.
Eric Topol (14:12):
So what you described, is it the same as a virtual cell? Is it kind of a precursor to it? How do you conceive this because this is such a complex, I mean it’s a fundamental unit of life, but it's also so much more complex than a protein or an RNA because not only all the things inside the cell, inside all these organelles and nucleus, but then there's all the outside interactions. So this is a bold challenge, right?
Anna Greka (14:41):
Oh my god, it's absolutely from a biologist perspective, it's the challenge of a generation for sure. We think taking humans to Mars, I mean that's an aspirational sort of big ambitious goal. I think this is the, if you will, the Mars shot for biology, being able to, whether the terminology, whether you call it a virtual cell. I like the idea of saying that to state it as a problem, the way that people who think about it from a mathematics perspective for example, would think about it. I think stating it as the cell prediction problem appeals to me because it actually forces us biologists to think about setting up the way that we would do these cell perturbation data sets, the way we would generate them to set them up to serve predictions. So for example, the way that I would think about this would be can I in the future have so much information about how cell perturbations work that I can train a model so that it can predict when I show it a picture of another cell under different conditions that it hasn't seen before, that it can still tell me, ah, this is a neuron in which you perturbed the mitochondria, for example, and now this is sort of the outcome that you would expect to see.
Anna Greka (16:08):
And so, to be able to have this ability to have a model that can have the ability to predict in silico what cells would look like after perturbation, I think that's sort of the way that I think about this problem. It is very far away from anything that exists today. But I think that the beginning starts, and this is one of the unique things about my institute, if I can say, we have a place where cell biologists, geneticists, mathematicians, machine learning experts, we all come together in the same place to really think and grapple with these problems. And of course we're very outward facing, interacting with scientists all across the world as well. But there's this sort of idea of bringing people into one institute where we can just think creatively about these big aspirational problems that we want to solve. I think this is one of the unique things about the ecosystem at the Broad Institute, which I'm proud to be a part of, and it is this kind of out of the box thinking that will hopefully get us to generate the kinds of data sets that will serve the needs of building these kinds of models with predictive capabilities down the road.
Anna Greka (17:19):
But as you astutely said, AlphaFold of course was based on the protein database existing, right? And that was a wealth of available information in which one could train models that would ultimately be predictive, as we have seen this miracle that Demi Hassabis and John Jumper have given to humanity, if you will.
Anna Greka (17:42):
But as Demis and John would also say, I believe is as I have discussed with them, in fact, the cell prediction problem is really a bigger problem because we do not have a protein data bank to go to right now, but we need to create it to generate these data. And so, my Ladders to Cures Accelerator is here to basically provide some part of the answer to that problem, create this kind of well-controlled database that we need for cell perturbations, while at the same time maximizing our learnings about these fully penetrant coding mutations and what their downstream sequelae would be in many different human cells. And so, in this way, I think we can both advance our knowledge about these monogenic diseases, build models, hopefully with predictive capabilities. And to your point, a lot of what we will learn about this biology, if we think that it involves 8,000 or more out of the 20,000 genes in our genome, it will of course serve our understanding of polygenic diseases ultimately as well as we go deeper into this biology and we look at the combinatorial aspects of what different mutations do to human cells. And so, it's a huge aspirational problem for a whole generation, but it's a good one to work on, I would say.
Learning the Language of Life with A.I.
Eric Topol (19:01):
Oh, absolutely. Now I think you already mentioned something that's quite, well, two things from what you just touched on. One of course, how vital it is to have this inner or transdisciplinary capability because you do need expertise across these vital areas. But the convergence, I mean, I love your term nodal biology and the fact that there's all these diseases like you were talking about, they do converge and nodal is a good term to highlight that, but it's not. Of course, as you mentioned, we have genome editing which allows to look at lots of different genome perturbations, like the single letter change that you found in MUC1 pathogenic critical mutation. There's also the AI world which is blossoming like I've never seen. In fact, I had in Science this week about learning the language of life with AI and how there's been like 15 new foundation models, DNA, proteins, RNA, ligands, all their interactions and the beginning of the cell story too with the human cell.
Eric Topol (20:14):
So this is exploding. As you said, the expertise in computer science and then this whole idea that you could take these powerful tools and do as you said, which is the need to accelerate, we just can't sit around here when there's so much discovery work to be done with the scalability, even though it might take years to get to this artificial intelligence virtual cell, which I have to agree, everyone in biology would say that's the holy grail. And as you remember at our conference in London, Demi Hassabis said that's what we'd like to do now. So it has the attention of leaders in AI around the world, obviously in the science and the biomedical community like you and many others. So it is an extraordinary time where we just can't sit still with these tools that we have, right?
Anna Greka (21:15):
Absolutely. And I think this is going to be, you mentioned the ASCI presidency in the beginning of our call. This is going to be the president gets to give an address at the annual meeting in Chicago. This is going to be one of the points I make, no matter what field in biomedicine we're in, we live in, I believe, a golden era and we have so many tools available to us that we can really accelerate our ability to help more patients. And of course, this is our mandate, the most important stakeholders for everything that we do as physician-scientists are our patients ultimately. So I feel very hopeful for the future and our ability to use these tools and to really make good on the promise of research is a public good. And I really hope that we can advance our knowledge for the benefit of all. And this is really an exciting time, I think, to be in this field and hopefully for the younger colleagues a time to really get excited about getting in there and getting involved and asking the big questions.
Career Reflections
Eric Topol (22:21):
Well, you are the prototype for this and an inspiration to everyone really, I'm sure to your lab group, which you highlighted in the TED Talk and many other things that you do. Now I want to spend a little bit of time about your career. I think it's fascinating that you grew up in Greece and your father's a nephrologist and your mother's a pathologist. So you had two physicians to model, but I guess you decided to go after nephrology, which is an area in medicine that I kind of liken it to Rodney Dangerfield, he doesn't get any respect. You don't see many people that go into nephrology. But before we get to your decision to do that somehow or other you came from Greece to Harvard for your undergrad. How did you make that connect to start your college education? And then subsequently you of course you stayed in Boston, you've never left Boston, I think.
Anna Greka (23:24):
I never left. Yeah, this is coming into 31 years now in Boston.
Anna Greka (23:29):
Yeah, I started as a Harvard undergraduate and I'm now a full professor. It's kind of a long, but wonderful road. Well, actually I would credit my parents. You mentioned that my father, they're both physician-scientists. My father is now both retired, but my father is a nephrologist, and my mother is a pathologist, actually, they were both academics. And so, when we were very young, we lived in England when my parents were doing postdoctoral work. That was actually a wonderful gift that they gave me because I became bilingual. It was a very young age, and so that allowed me to have this advantage of being fluent in English. And then when we moved back to Greece where I grew up, I went to an American school. And from that time, this is actually an interesting story in itself. I'm very proud of this school.
Anna Greka (24:22):
It's called Anatolia, and it was founded by American missionaries from Williams College a long time ago, 150 and more years ago. But it is in Thessaloniki, Greece, which is my hometown, and it's a wonderful institution, which gave me a lot of gifts as well, preparing me for coming to college in the United States. And of course, I was a good student in high school, but what really was catalytic was that I was lucky enough to get a scholarship to go to Harvard. And that was really, you could say the catalyst that propelled me from a teenager who was dreaming about a career as a physician-scientist because I certainly was for as far back as I remember in fact. But then to make that a reality, I found myself on the Harvard campus initially for college, and then I was in the combined Harvard-MIT program for my MD PhD. And then I trained in Boston at Mass General in Brigham, and then sort of started my academic career. And that sort of brings us to today, but it is an unlikely story and one that I feel still very lucky and blessed to have had these opportunities. So for sure, it's been wonderful.
Eric Topol (25:35):
We're the ones lucky that you came here and set up shop and you did your productivity and discovery work and sleuthing has been incredible. But I do think it's interesting too, because when you did your PhD, it was in neuroscience.
Anna Greka (25:52):
Ah, yes. That's another.
Eric Topol (25:54):
And then you switch gears. So tell us about that?
Anna Greka (25:57):
This is interesting, and actually I encourage more colleagues to think about it this way. So I have always been driven by the science, and I think that it seems a little backward to some people, but I did my PhD in neuroscience because I was interested in understanding something about these ion channels that were newly discovered at the time, and they were most highly expressed in the brain. So here I was doing work in the brain in the neuroscience program at Harvard, but then once I completed my PhD and I was in the middle of my residency training actually at Mass General, I distinctly remember that there was a paper that came out that implicated the same family of ion channels that I had spent my time understanding in the brain. It turned out to be a channelopathy that causes kidney disease.
Anna Greka (26:43):
So that was the light bulb, and it made me realize that maybe what I really wanted to do is just follow this thread. And my scientific curiosity basically led me into studying the kidney and then it seemed practical therefore to get done with my clinical training as efficiently as possible. So I finished residency, I did nephrology training, and then there I was in the lab trying to understand the biology around this channelopathy. And that sort of led us into the early projects in my young lab. And in fact, it's interesting we didn't talk about that work, but that work in itself actually has made it all the way to phase II trials in patients. This was a paper we published in Science in 2017 and follow onto that work, there was an opportunity to build this into a real drug targeting one of these ion channels that has made it into phase II trials. And we'll see what happens next. But it's this idea of following your scientific curiosity, which I also talked about in my TED Talk, because you don't know to what wonderful places it will lead you. And quite interestingly now my lab is back into studying familial Alzheimer's and retinitis pigmentosa in the eye in brain. So I tell people, do not limit yourself to whatever someone says your field is or should be. Just follow your scientific curiosity and usually that takes you to a lot more interesting places. And so, that's certainly been a theme from my career, I would say.
Eric Topol (28:14):
No, I think that's perfect. Curiosity driven science is not the term. You often hear hypothesis driven or now with AI you hear more AI exploratory science. But no, that's great. Now I want to get a little back to the AI story because it’s so fascinating. You use lots of different types of AI such as cellular imaging would be fusion models and drug discovery. I mean, you've had drug discovery for different pathways. You mentioned of course the ion channel and then also as we touched on with your Cell paper, the whole idea of targeting the cargo receptor with a small molecule and then things in between. You discussed this of course at the London panel, but maybe you just give us the skinny on the different ways that you incorporate AI in the state-of-the-art science that you're doing?
Anna Greka (29:17):
Sure, yeah, thank you. I think there are many ways in which even for quite a long time before AI became such a well-known kind of household term, if you will, the concept of machine learning in terms of image processing is something that has been around for some time. And so, this is actually a form of AI that we use in order to process millions of images. My lab has by produced probably more than 20 million images over the last few years, maybe five to six years. And so, if you can imagine it's impossible for any human to process this many images and make sense of them. So of course, we've been using machine learning that is becoming increasingly more and more sophisticated and advanced in terms of being able to do analysis of images, which is a lot of what we cell biologists do, of course.
Anna Greka (30:06):
And so, there's multiple different kinds of perturbations that we do to cells, whether we're using CRISPR or base editing to make, for example, genome wide or genome scale perturbations or small molecules as we have done as well in the past. These are all ways in which we are then using machine learning to read out the effects in images of cells that we're looking at. So that's one way in which machine learning is used in our daily work, of course, because we study misshape and mangled proteins and how they are recognized by these cargo receptors. We also use AlphaFold pretty much every day in my lab. And this has been catalytic for us as a tool because we really are able to accelerate our discoveries in ways that were even just three or four years ago, completely impossible. So it's been incredible to see how the young people in my lab are just so excited to use these tools and they're becoming extremely savvy in using these tools.
Anna Greka (31:06):
Of course, this is a new generation of scientists, and so we use AlphaFold all the time. And this also has a lot of implications of course for some of the interventions that we might think about. So where in this cargo receptor complex that we study for example, might we be able to fit a drug that would disrupt the complex and lead the cargo tracks into the lysosome for degradation, for example. So there's many ways in which AI can be used for all of these functions. So I would say that if we were to organize our thinking around it, one way to think about the use of machine learning AI is around what I would call understanding biology in cells and what in sort of more kind of drug discovery terms you would call target identification, trying to understand the things that we might want to intervene on in order to have a benefit for disease.
Anna Greka (31:59):
So target ID is one area in which I think machine learning and AI will have a catalytic effect as they already are. The other of course, is in the actual development of the appropriate drugs in a rational way. So rational drug design is incredibly enabled by AlphaFold and all these advances in terms of understanding protein structures and how to fit drugs into them of all different modalities and kinds. And I think an area that we are not yet harnessing in my group, but I think the Ladders to Cures Accelerator hopes to build on is really patient data. I think that there's a lot of opportunity for AI to be used to make sense of medical records for example and how we extract information that would tell us that this cohort of patients is a better cohort to enroll in your trial versus another. There are many ways in which we can make use of these tools. Not all of them are there yet, but I think it's an exciting time for being involved in this kind of work.
Eric Topol (32:58):
Oh, no question. Now it must be tough when you know the mechanism of these families disease and you even have a drug candidate, but that it takes so long to go from that to helping these families. And what are your thoughts about that, I mean, are you thinking also about genome editing for some of these diseases or are you thinking to go through the route of here's a small molecule, here's the tox data in animal models and here's phase I and on and on. Where do you think because when you know so much and then these people are suffering, how do you bridge that gap?
Anna Greka (33:39):
Yeah, I think that's an excellent question. Of course, having patients as our partners in our research is incredible as a way for us to understand the disease, to build biomarkers, but it is also exactly creating this kind of emotional conflict, if you will, because of course, to me, honesty is the best policy, if you will. And so, I'm always very honest with patients and their families. I welcome them to the lab so they can see just how long it takes to get some of these things done. Even today with all the tools that we have, of course there are certain things that are still quite slow to do. And even if you have a perfect drug that looks like it fits into the right pocket, there may still be some toxicity, there may be other setbacks. And so, I try to be very honest with patients about the road that we're on. The small molecule path for the toxic proteinopathies is on its way now.
Anna Greka (34:34):
It's partnered with a pharmaceutical company, so it's on its way hopefully to patients. Of course, again, this is an unpredictable road. Things can happen as you very well know, but I'm at least glad that it's sort of making its way there. But to your point, and I'm in an institute where CRISPR was discovered, and base editing and prime editing were discovered by my colleagues here. So we are in fact looking at every other modality that could help with these diseases. We have several hurdles to overcome because in contrast to the liver and the brain, the kidney for example, is not an organ in which you can easily deliver nucleic acid therapies, but we're making progress. I have a whole subgroup within the bigger group who's focusing on this. It's actually organized in a way where they're running kind of independently from the cell biology group that I run.
Anna Greka (35:31):
And it's headed by a person who came from industry so that she has the opportunity to really drive the project the way that it would be run milestone driven, if you will, in a way that it would be run as a therapeutics program. And we're really trying to go after all kinds of different nucleic acid therapies that would target the mutations themselves rather than the cargo receptors. And so, there's ASO and siRNA technologies and then also actual gene editing technologies that we are investigating. But I would say that some of them are closer than others. And again, to your question about patients, I tell them honestly when a project looks to be more promising, and I also tell them when a project looks to have hurdles and that it will take long and that sometimes I just don't know how long it will take before we can get there. The only thing that I can promise patients in any of our projects, whether it's Alzheimer's, blindness, kidney disease, all I can promise is that we're working the hardest we possibly can on the problem.
Anna Greka (36:34):
And I think that is often reassuring I have found to patients, and it's best to be honest about the fact that these things take a long time, but I do think that they find it reassuring that someone is on it essentially, and that there will be some progress as we move forward. And we've made progress in the very first discovery that came out of my lab. As I mentioned to you, we've made it all the way to phase II trials. So I have seen the trajectory be realized, and I'm eager to make it happen again and again as many times as I can within my career to help as many people as possible.
The Paucity of Physician-Scientists
Eric Topol (37:13):
I have no doubts that you'll be doing this many times in your career. No, there's no question about it. It's extraordinary actually. There's a couple of things there I want to pick up on. Physician-scientists, as you know, are a rarefied species. And you have actually so nicely told the story about when you have a physician-scientist, you're caring for the patients that you're researching, which is, most of the time we have scientists. Nothing wrong with them of course, but you have this hinge point, which is really important because you’re really hearing the stories and experiencing the patients and as you say, communicating about the likelihood of being able to come up with a treatment or the progress. What are we going to do to get more physician-scientists? Because this is a huge problem, it has been for decades, but the numbers just keep going lower and lower.
Anna Greka (38:15):
I think you're absolutely right. And this is again, something that in my leadership of the ASCI I have made sort of a cornerstone of our efforts. I think that it has been well-documented as a problem. I think that the pressures of modern clinical care are really antithetical to the needs of research, protected time to really be able to think and be creative and even have the funding available to be able to pursue one's program. I think those pressures are becoming so heavy for investigators that many of them kind of choose one or the other route most often the clinical route because that tends to be, of course where they can support their families better. And so, this has been kind of the conundrum in some ways that we take our best and brightest medical students who are interested in investigation, we train them and invest in them in becoming physician-scientists, but then we sort of drop them at the most vulnerable time, which is usually after one completes their clinical and scientific training.
Anna Greka (39:24):
And they're embarking on early phases of one's careers. It has been found to be a very vulnerable point when a lot of people are now in their mid-thirties or even late thirties perhaps with some family to take care of other burdens of adulthood, if you will. And I think what it becomes very difficult to sustain a career where one salary is very limited due to the research component. And so, I think we have to invest in our youngest people, and it is a real issue that there's no good mechanism to do that at the present time. So I was actually really hoping that there would be an opportunity with leadership at the NIH to really think about this. It's also been discussed at the level of the National Academy of Medicine where I had some role in discussing the recent report that they put out on the biomedical enterprise in the United States. And it's kind of interesting to see that there is a note made there about this issue and the fact that there needs to be, I think, more generous investment in the careers of a few select physician-scientists that we can support. So if you look at the numbers, currently out of the entire physician workforce, a physician-scientist comprised of less than 1%.
Anna Greka (40:45):
It’s probably closer to 0.8% at this point.
Eric Topol (40:46):
No, it's incredible.
Anna Greka (40:48):
So that's really not enough, I think, to maintain the enterprise and if you will, this incredible innovation economy that the United States has had this miracle engine, if you will, in biomedicine that has been fueled in large part by physician investigators. Of course, our colleagues who are non-physician investigators are equally important partners in this journey. But we do need a few of the physician-scientists investigators I think as well, if you really think about the fact that I think 70% of people who run R&D programs in all the big pharmaceutical companies are physician-scientists. And so, we need people like us to be able to work on these big problems. And so, more investment, I think that the government, the NIH has a role to play there of course. And this is important from both an economic perspective, a competition perspective with other nations around the world who are actually heavily investing in the physician-scientist workforce.
Anna Greka (41:51):
And I think it's also important to do so through our smaller scale efforts at the ASCI. So one of the things that I have been involved in as a council member and now as president is the creation of an awards program for those early career investigators. So we call them the Emerging-Generation Awards, and we also have the Young Physician-Scientist Awards. And these are really to recognize people who are making that transition from being kind of a trainee and a postdoc and have finished their clinical training into becoming an independent assistant professor. And so, those are small awards, but they're kind of a symbolic tap on the shoulder, if you will, that the ASCI sees you, you're talented, stay the course. We want you to become a future member. Don't give up and please keep on fighting. I think that can take us only so far.
Anna Greka (42:45):
I mean, unless there's a real investment, of course still it will be hard to maintain people in the pipeline. But this is just one way in which we have tried to, these programs that the ASCI offers have been very successful over the last few years. We create a cohort of investigators who are clearly recognized by members of the ASCI is being promising young colleagues. And we give them longitudinal training as part of a cohort where they learn about how to write a grant, how to write a paper, leadership skills, how to run a lab. And they're sort of like a buddy system as well. So they know that they're in it together rather than feeling isolated and struggling to get their careers going. And so, we've seen a lot of success. One way that we measure that is conversion into an ASCI membership. And so, we're encouraged by that, and we hope that the program can continue. And of course, as president, I'm going to be fundraising for that as well, it's part of the role. But it is a really worthy cause because to your point, we have to somehow make sure that our younger colleagues stay the course that we can at least maintain, if not bolster our numbers within the scientific workforce.
Eric Topol (43:57):
Well, you outlined some really nice strategies and plans. It's a formidable challenge, of course. And we'd like to see billions of dollars to support this. And maybe someday we will because as you say, if we could relieve the financial concerns of people who have curiosity driven ideas.
Anna Greka (44:18):
Exactly.
Eric Topol (44:19):
We could do a lot to replenish and build a big physician-scientist workforce. Now, the last thing I want to get to, is you have great communication skills. Obviously, anybody who is listening or watching this.
Eric Topol (44:36):
Which is another really important part of being a scientist, no less a physician or the hybrid of the two. But I wanted to just go to the backstory because your TED Talk, which has been watched by hundreds of thousands of people, and I'm sure there's hundreds of thousands more that will watch it, but the TED organization is famous for making people come to the place a week ahead. This is Vancouver used to be in LA or Los Angeles area and making them rehearse the talk, rehearse, rehearse, rehearse, which seems crazy. You could train the people there, how to give a talk. Did you have to go through that?
Anna Greka (45:21):
Not really. I did rehearse once on stage before I actually delivered the talk live. And I was very encouraged by the fact that the TED folks who are of course very well calibrated, said just like that. It's great, just like that.
Eric Topol (45:37):
That says a lot because a lot of people that do these talks, they have to do it 10 times. So that kind of was another metric. But what I don't like about that is it just because these people almost have to memorize their talks from giving it so much and all this coaching, it comes across kind of stilted and unnatural, and you're just a natural great communicator added to all your other things.
Anna Greka (46:03):
I think it’s interesting. Actually, I would say, if I may, that I credit, of course, I actually think that it's important, for us physician-scientists, again, science and research is a public good, and being able to communicate to the public what it is that we do, I think is kind of an obligation for the fact that we are funded by the public to do this kind of work. And so, I think that's important. And I always wanted to cultivate those communication skills for the benefit of communicating simply and clearly what it is that we do in our labs. But also, I would say as part of my story, I mentioned that I had the opportunity to attend a special school growing up in Greece, Anatolia, which was an American school. One of the interesting things about that is that there was an oratory competition.
Anna Greka (46:50):
I got very early exposure entering that competition. And if you won the first prize, it was in the kind of ancient Rome way, first among equals, right? And so, that was the prize. And I was lucky to have this early exposure. This is when I was 14, 15, 16 years old, that I was training to give these oratory speeches in front of an audience and sort of compete with other kids who were doing the same. I think these are just wonderful gifts that a school can give a student that have stayed with me for life. And I think that that's a wonderful, yeah, I credit that experience for a lot of my subsequent capabilities in this area.
Eric Topol (47:40):
Oh, that's fantastic. Well, this has been such an enjoyable conversation, Anna. Did I miss anything that we need to bring up, or do you think we have it covered?
Anna Greka (47:50):
Not at all. No, this was wonderful, and I thoroughly enjoyed it as well. I'm very honored seeing how many other incredible colleagues you've had on the show. It's just a great honor to be a part of this. So thank you for having me.
Eric Topol (48:05):
Well, you really are such a great inspiration to all of us in the biomedical community, and we'll be cheering for your continued success and thanks so much for joining today, and I look forward to the next time we get a chance to visit.
Anna Greka (48:20):
Absolutely. Thank you, Eric.
**************************************
Thanks for listening, watching or reading Ground Truths. Your subscription is greatly appreciated.
If you found this podcast interesting please share it!
That makes the work involved in putting these together especially worthwhile.
All content on Ground Truths—newsletters, analyses, and podcasts—is free, open-access.
Paid subscriptions are voluntary and all proceeds from them go to support Scripps Research. They do allow for posting comments and questions, which I do my best to respond to.
Many thanks to those who have contributed—they have greatly helped fund our summer internship programs for the past two years. And such support is becoming more vital In light of current changes of funding and support for biomedical research at NIH and other US governmental agencies.
Thanks to my producer Jessica Nguyen and to Sinjun Balabanoff for audio and video support at Scripps Research.












Share this post